Abstract
MAFLD is highly prevalent among overweight and obese individuals. Recently, the American Heart Association proposed a new measure of cardiovascular health (Life’s Essential 8). This study investigated the relationship between the Life’s Essential 8 (LE8) and MAFLD, all-cause and cardiovascular mortality in these populations, exploring the mediating role of inflammation and insulin resistance. This retrospective study used data from the National Health and Nutrition Examination Survey (NHANES, 2007–2018), including 6,885 overweight and obese individuals. LE8 scores were categorized into low, medium, and high groups. Weighted logistic regression and Cox proportional hazards models assessed the relationships between LE8, MAFLD, and mortality. Mediation analyses explored the roles of inflammation and insulin resistance, and weighted restricted cubic spline (RCS) regression examined potential nonlinear associations. Kaplan-Meier survival analysis evaluated survival rates across LE8 groups, and subgroup analyses assessed interactions with demographic characteristics. Additionally, ROC curves were used to explore the predictive accuracy of various inflammation and insulin resistance biomarkers. In model 3, compared to the low LE8 group, the prevalence of MAFLD in the highest LE8 group was reduced by 89% (OR = 0.11; 95% CI: 0.06, 0.20). HOMA-IR mediated 72.26% of the mediation effect. Various inflammation markers, including CRP, hs-CRP, SII, and SIRI indices, mediated effects ranging from 3 to 12%. Compared to the low LE8 group, the highest LE8 group had a 58% reduction in all-cause mortality and a 90% reduction in cardiovascular mortality. Kaplan-Meier analysis showed that the higher LE8 groups had significantly higher survival rates than the low LE8 group. Inflammatory markers mediated 5-17% of the mediation effects. Restricted cubic spline (RCS) curves revealed a non-linear relationship between LE8 and MAFLD. Age interacted with LE8 in several subgroup analyses. ROC curves showed that HOMA-IR had strong predictive accuracy for MAFLD, while SIRI demonstrated potential advantages in predicting mortality risk. In overweight/obese populations, LE8 scores were negatively associated with the prevalence of MAFLD, and risk of mortality. These findings emphasize the importance of maintaining high levels of LE8 scores for primary prevention in overweight/obese populations.
Similar content being viewed by others
Introduction
The prevalence of non-alcoholic fatty liver disease (NAFLD) is 25% in the general population1, but it is approximately 70% among overweight and obese individuals2. NAFLD is the most common liver disease in obese populations and can progress to more severe liver conditions, such as non-alcoholic steatohepatitis (NASH), liver fibrosis, and cirrhosis3. However, the clinical diagnosis of NAFLD is a process of exclusion, requiring the elimination of alcohol consumption and other causes of hepatic steatosis or steatohepatitis, which complicates its diagnosis. In 2020, an international expert panel proposed redefining and renaming NAFLD as metabolic dysfunction-associated fatty liver disease (MAFLD) to more accurately reflect the relationship between fatty liver and metabolic dysfunction4. The updated MAFLD diagnostic criteria take a positive diagnostic approach and are considered more effective in identifying high-risk liver diseases, extrahepatic complications, metabolic dysfunction, and in predicting liver fibrosis. Inflammation and insulin resistance are key pathological processes in the development and progression of MAFLD5. Chronic low-grade inflammation contributes to hepatic steatosis and fibrosis through the activation of pro-inflammatory cytokines and immune cells, while insulin resistance promotes lipid accumulation and impairs glucose metabolism in hepatocytes5,6,7. Thus, improving inflammation and insulin resistance is considered one of the most effective strategies for preventing and managing MAFLD. Additionally, obese individuals face a higher risk of all-cause and cardiovascular mortality compared to those with normal weight. The increased prevalence of MAFLD and associated mortality places a significant burden on the overweight and obese population, highlighting the importance of effective health management for this group.
In 2022, the American Heart Association introduced a new metric for cardiovascular health, Life’s Essential 8 (LE8)8. Its predecessor, LE7, has been recognized as an important tool for primary prevention in healthcare systems9, demonstrating protective effects against cardiovascular and other chronic diseases. LE8 expands upon LE7 by incorporating sleep quality and a revised algorithm. It includes eight components: diet, physical activity, nicotine exposure, body mass index (BMI), blood pressure, blood glucose levels, cholesterol levels, and sleep health8,10. Higher LE8 scores are associated with better cardiovascular health and lower risks of cardiovascular mortality11. However, the relationship between LE8 and MAFLD, as well as mortality risks in overweight and obese populations, remains inadequately studied.
In our study, we utilized the traditional biomarker HOMA-IR (homeostasis model assessment of insulin resistance) to assess insulin resistance12. To evaluate systemic inflammation, we employed classic inflammatory markers, including CRP, the CRP/albumin ratio, and ferritin. Additionally, we incorporated two novel inflammatory indices, SII (systemic immune-inflammation index) and SIRI (systemic inflammation response index), to provide further insights. SII is calculated by platelet count*neutrophil count/lymphocyte count, while SIRI is derived from monocyte*neutrophil/lymphocyte count13,14. These indices reflect three critical pathways: inflammation, thrombosis, and adaptive immunity, all of which are closely associated with the pathogenesis of MAFLD15,16,17. Several population-based studies have demonstrated a positive correlation between SII, SIRI, and both the risk of developing NAFLD/MAFLD and mortality associated with the disease18,19,20. Additionally, it is well-established that inflammatory indices are generally elevated in obese populations21. These risks of inflammation may lead to a variety of adverse outcomes in overweight/obese populations.
Utilizing data from the National Health and Nutrition Examination Survey (NHANES)22, this study examined the association between LE8 and the prevalence of MAFLD, along with its relationship to all-cause and cardiovascular mortality in overweight and obese individuals. Additionally, the mediating roles of inflammation and insulin resistance in these associations were evaluated. By incorporating both traditional and novel inflammatory and metabolic markers, our study aimed to provide insights into the potential mechanisms of LE8 and offer a basis for developing preventive strategies tailored to this population.
Method
Research design
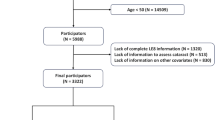
The National Health and Nutrition Examination Survey (NHANES) is an essential program that monitors the health and nutritional status of the U.S. population22. It employs a sophisticated, multistage sampling design to ensure representation from diverse demographic groups. NHANES collects comprehensive data on demographics, dietary habits, medical history, as well as physical and laboratory assessments, making it an invaluable resource for tracking public health trends and informing policy decisions. All participants provide informed consent, and the survey’s protocols undergo rigorous ethical review. Detailed methodologies and data from NHANES are publicly available on the official website. The combined cycles from 2007 to 2018 included 59,842 participants. The sample pool excluded individuals with missing data on LE8, US-FLI, BMI < 25, pregnant women, and other ineligible participants. The final sample size for this study was 6,885 individuals. Figure 1 provides a flowchart outlining the study selection process and research design.
Assessment of life’s essential 8(LE8)
The LE8 score consists of 4 health factors—body mass index, lipids, blood glucose, and blood pressure—and 4 health behaviors—diet, physical activity, nicotine exposure, and sleep health. The specific calculations of LE8 are detailed in Supplementary Table 1. The LE8 score ranges from 0 to 100, with the total LE8 score being the mean of the 8 indicators. LE8 scores are categorized as follows: 80–100 as high, 50–79 as moderate, and 0–49 as low23,24,25.
The dietary indicator was assessed using the HEI-2015 index26, which was calculated from dietary intake data obtained through two 24-hour dietary recall questionnaires26,27,28. Data on smoking, sleep, physical activity, and medication use were collected through NHANES questionnaires. Physical examinations measured BMI and blood pressure, while laboratory tests assessed lipids, blood glucose, and glycosylated hemoglobin levels29.
Assessment of MAFLD and NAFLD
US-FLI was used to assess for hepatic steatosis30.
Participants were assigned a value of 1 if they identified as Non-Hispanic Black or Mexican American, and 0 if they did not. Based on previous studies, participants with a US-FLI ≥ 30 were classified as having hepatic steatosis. MAFLD was defined by the presence of liver steatosis and at least one of the following conditions: (1) overweight or obesity, defined as BMI ≥ 25 kg/m²; (2) type 2 diabetes; or (3) evidence of at least two metabolic risk factors. These risk factors included: (1) waist circumference ≥ 102/88 cm for men and women, respectively; (2) blood pressure ≥ 130/85 mmHg or use of antihypertensive medication; (3) plasma triglycerides ≥ 150 mg/dl or use of specific medications; (4) low HDL cholesterol levels (HDL < 40 mg/dl for men, HDL < 50 mg/dl for women) or use of specific medications; (5) prediabetes (fasting glucose 100–125 mg/dl or HbA1c 5.7–6.4%); (6) HOMA-IR ≥ 2.5; or (7) hs-CRP > 2 mg/L31. NAFLD is diagnosed based on the presence of liver steatosis and the exclusion of chronic hepatitis factors, including hepatitis B surface antigen, hepatitis C antibody or RNA, and heavy alcohol consumption (≥ 2 drinks per day for men or ≥ 1 drink per day for women)32,33.
All-cause mortality and cardiovascular mortality
Mortality data were obtained by linking NHANES participant information to death certificate records from the National Death Index (NDI), with data available through December 31, 2019. Cardiovascular mortality was identified using death codes (I00-I09, I11, I13, I20-I51, and I60-I69)34.
Inflammation and insulin resistance index
Due to the characteristics of NHANES data collection, CRP data are available for the NHANES (2007–2010) cycle, while hs-CRP data are from the NHANES (2015–2018) cycle. The NHANES (2011–2014) cycle did not include CRP/hs-CRP data. Ferritin data are available for both NHANES (2007–2010) and (2015–2018). Specifically, NHANES (2007–2010, 2015–2016) collected data from all participants aged 1–5 years and women aged 12–49 years, while NHANES (2017–2018) collected data from all participants aged 1–5 years and those aged 12 years and older. Albumin, blood glucose, and blood cell counts were measured across all study periods.
HOMA-IR is commonly used to predict insulin resistance and is based on the relationship between glucose and insulin dynamics under fasting conditions. It is calculated as: fasting insulin (mU/dL) × fasting glucose (mmol/L)/22.535. SII and SIRI are derived from a combination of blood cell counts. SII is calculated as platelet count × neutrophil count/lymphocyte count, while SIRI is calculated as neutrophil count × monocyte count/lymphocyte count13,14. Both SII and SIRI are used to assess systemic immune-inflammation.
Covariates
Potential confounding factors were considered in our analysis depending, including age, race, sex, marriage, education, family income-to-poverty ratio(PIR), alcohol intake, hypertension36, ALT, AST, triglyceride, and fasting glucose. Education levels were categorized as </=/> high school. Marital status was categorized as living alone, partnered, and married. Ethnicity was grouped into five categories: non-Hispanic white, non-Hispanic black, Mexican American, other Hispanic, and other race. The PIR, an index used to assess a household’s socio-economic position, was divided into three categories: <1.5, 1.5–3.5, and > 3.5. Hypertension was defined as physician-diagnosed high blood pressure, use of antihypertensive medications, or average systolic blood pressure > 140 mmHg or diastolic > 90 mmHg. BMI was used to classify individuals into overweight or obese categories according to WHO criteria.
Statistical analysis
Sample weights were applied in all analyses to account for the complex sampling design of the NHANES study. Continuous variables were presented as weighted means with standard deviations, while categorical variables were expressed as unweighted frequencies alongside their corresponding weighted frequencies. For comparing between-group differences, the Kruskal-Wallis test was used for continuous variables, and the Chi-square test was applied for categorical variables. The associations between LE8, MAFLD, and mortality were evaluated using multifactorial logistic regression and Cox proportional hazards models. Additionally, weighted restricted cubic spline (RCS) regression was employed to assess the potential nonlinear relationships between LE8, MAFLD, and mortality. The analyses were also stratified by age, sex, ethnicity, marital status, educational background, income, and hypertension, with interaction tests used to assess the presence of subgroups for dependence. Although all covariates were adjusted for in the multivariable models, stratified analysis allows for a more nuanced examination of how LE8’s effects may vary across different subgroups. This approach helps identify potential effect modifications and provides a deeper understanding of LE8’s impact across diverse demographic groups. By considering these subgroup differences, we can better appreciate how LE8 may benefit populations with distinct characteristics.
Kaplan-Meier curves were generated to assess survival probabilities at different LE8 levels. Mediation analysis was conducted using the R package “mediation,†which is widely recognized for its application in such analyses37,38,39,40. As illustrated in the flow diagram of Fig. 2, LE8 was used as the exposure (X), with MAFLD and mortality risk as the outcomes (Y). The Inflammation and insulin resistance index served as mediators. The proportion of the total effect mediated through the pathway X → M → Y was examined41. R software 4.2.3 was utilized to perform all of the aforementioned analyses.
Result
Basic features of participants
The study comprised 6,885 participants in total, 1,579 with low LE8 (0–49), 4,890 with intermediate LE8 (50–79), and 416 with high LE8 (80–100). A total of 3,233 participants (46%) were diagnosed with MAFLD, a result similar to that found in a previous epidemiological study42. In contrast, 1,458 participants (18%) were diagnosed with NAFLD. Additionally, 1,775 participants were diagnosed with MAFLD but not NAFLD. One of the main reasons for this significant difference is the inclusion of alcohol consumption criteria in the NAFLD definition. Furthermore, US-FLI scores were higher in the low LE8 group than the high LE8 group. Those with higher LE8 scores were also characterized as younger, non-Hispanic white, married status, higher education, higher income level, and no history of hypertension. All characteristics are detailed in Table 1.
Relationship between LE8 and MAFLD and NAFLD
As shown in Table 2, weighted logistic regression revealed that LE8 was negatively associated with both MAFLD and NAFLD (P < 0.05). In the fully adjusted model, for each 10-point increase in the LE8 score, the odds of MAFLD decreased significantly (OR = 0.59; 95% CI = (0.55, 0.64); P < 0.001). The prevalence of MAFLD was 53% and 89% lower in the intermediate LE8 (OR = 0.47; 95% CI = (0.37, 0.58); P < 0.001) and high LE8 groups (OR = 0.11; 95% CI = (0.06, 0.20); P < 0.001), respectively, compared with the low LE8 group. Similarly, for NAFLD, the odds of prevalence decreased by 35% and 82% in the intermediate LE8 (OR = 0.65; 95% CI = (0.49, 0.87); P < 0.001) and high LE8 groups (OR = 0.18; 95% CI = (0.08, 0.38); P < 0.001), respectively, relative to the low LE8 group.
Relationship of LE8 with mortality
During a median follow-up of 80 months, we found that LE8 was inversely associated with the risk of all-cause and cardiovascular mortality. In Table 3, compared with the low LE8 group, the intermediate LE8 group showed a 31% reduction in the risk of all-cause mortality (HR = 0.69; 95% CI: 0.55–0.88; P = 0.002), while the high LE8 group experienced a 58% reduction (HR = 0.42; 95% CI: 0.20–0.88; P = 0.022). For cardiovascular mortality, the high and intermediate LE8 groups had a 42% (HR = 0.58; 95% CI: 0.36–0.92; P = 0.020) and 90% (HR = 0.10; 95% CI: 0.02–0.64; P = 0.014) reduction in risk, respectively. Kaplan-Meier survival analysis demonstrated significantly higher survival rates in the higher and intermediate LE8 groups compared to the low LE8 group (log-rank test P < 0.0001) (Fig. 3).
Nonlinear correlation of LE8 with MAFLD and mortality
Figure 4A displays the RCS curves showing the relationship between LE8 and MAFLD, while Fig. 4B presents the results stratified by gender. They revealed a non-linear negative correlation between LE8 and MAFLD (P < 0.05 for nonlinearity). These curves suggest that the benefits increase progressively as the LE8 score rises, with a greater magnitude of benefit observed at higher scores. Figure 4C and D illustrate the linear relationship (P > 0.05 for nonlinearity) between LE8 and the risks of all-cause and cardiovascular mortality, respectively.
The relationship between inflammation, insulin resistance, MAFLD, and mortality
As shown in Table 4, logistic regression analysis revealed significant positive associations between several markers and the prevalence of MAFLD in the overweight/obese population. Specifically, Ln(SII) was positively associated with the prevalence of MAFLD (OR = 1.34, 95% CI: 1.14–1.58, P < 0.001) in Model 3, as was Ln(SIRI) (OR = 1.41, 95% CI: 1.20–1.65, P < 0.001). HOMA-IR demonstrated a stronger positive association with MAFLD prevalence (OR = 6.92, 95% CI: 6.13–7.86, P < 0.001). Similarly, CRP (OR = 2.13, 95% CI: 1.65–2.82, P < 0.001) and CRP/albumin ratio (OR = 18.8, 95% CI: 6.84–57.0, P < 0.001) were also significantly associated with MAFLD prevalence. Additionally, hs-CRP (OR = 1.08, 95% CI: 1.05–1.10, P < 0.001) and hs-CRP/albumin ratio (OR = 1.33, 95% CI: 1.21–1.47, P < 0.001) demonstrated positive relationships with MAFLD. Ferritin showed no statistically significant association with MAFLD (OR = 1.00, 95% CI: 1.00–1.00, P = 0.672).
As shown in Supplementary Table 2, Cox regression analysis revealed that Ln(SII) was positively associated with all-cause mortality (HR = 1.28, 95% CI: 1.10–1.48, P < 0.001) in Model 3, as was Ln(SIRI) (HR = 1.60, 95% CI: 1.38–1.85, P < 0.001). CRP (HR = 1.21, 95% CI: 1.09–1.35, P < 0.001) and CRP/albumin ratio (HR = 2.13, 95% CI: 1.45–3.12, P < 0.001) also demonstrated significant positive associations with all-cause mortality. In contrast, HOMA-IR, hs-CRP, hs-CRP/albumin ratio, and ferritin were not significantly associated with all-cause mortality in Model 3.
As shown in the Supplementary Table 3, Cox regression analysis revealed that Ln(SII) was positively associated with cardiovascular mortality (HR = 1.72, 95% CI: 1.32–2.26, P < 0.001) in Model 3, as was Ln(SIRI) (HR = 1.89, 95% CI: 1.45–2.47, P < 0.001). CRP (HR = 1.25, 95% CI: 1.05–1.49, P = 0.012), CRP/albumin ratio (HR = 2.46, 95% CI: 1.34–4.49, P = 0.003), hs-CRP (HR = 1.04, 95% CI: 0.99–1.10, P = 0.094) and hs-CRP/albumin ratio (HR = 1.19, 95% CI: 0.98–1.45, P = 0.076) demonstrated positive associations with cardiovascular mortality, but the associations were not statistically significant at the 0.05 level. In contrast, HOMA-IR, and ferritin were not significantly associated with cardiovascular mortality in Model 3.
Additionally, The ROC curve analysis showed that HOMA-IR had the highest predictive value for MAFLD (AUC > 0.90) in Fig. 5. In contrast, inflammatory markers, including CRP/hs-CRP, CRP/Albumin, hs-CRP/Albumin, Ln(SII), and Ln(SIRI), showed weaker predictive performance(Fig. 5). Figure 6 shows ROC curves of different inflammatory markers in relation to mortality risk. For all-cause mortality, Ln(SIRI) (Fig. 6B and J) exhibited better predictive performance compared to Ln(SII) (Fig. 6A and I), CRP (Fig. 6C), CRP/Albumin (Fig. 6D), hs-CRP(Fig. 6K), and hs-CRP/Albumin(Fig. 6L). Similarly, for cardiovascular mortality, Ln(SIRI) (Fig. 6F and N) showed superior predictive value. These results underscore the potential utility of Ln(SIRI) as a robust marker for mortality risk prediction for Overweight and Obese Populations.
(A)ROC Curves of Ln(SII) for all-mortality risk in NHANES(2007–2010); (B)ROC curve of ln(SIRI) for all-mortality risk in NHANES(2007–2010); (C)ROC curve of CRP for all-mortality risk in NHANES(2007–2010); (D)ROC curve of CRP/Albumin for all-mortality risk in NHANES(2007–2010); (E)ROC curve of ln(SII) for cardiovascular mortality risk in NHANES(2007–2010); (F)ROC curve of ln(SIRI) for cardiovascular mortality risk in NHANES(2007–2010); (G)ROC curve of CRP for cardiovascular mortality risk in NHANES(2007–2010); (H)ROC curve of CRP/Albumin for cardiovascular mortality risk in NHANES(2007–2010).
(I)ROC Curves of Ln(SII) for all-mortality risk in NHANES(2015–2018); (J)ROC curve of ln(SIRI) for all-mortality risk in NHANES(2015–2018); (K)ROC curve of CRP for all-mortality risk in NHANES(2015–2018); (L)ROC curve of CRP/Albumin for all-mortality risk in NHANES(2015–2018); (M)ROC curve of ln(SII) for cardiovascular mortality risk in NHANES(2015–2018); (N)ROC curve of ln(SIRI) for cardiovascular mortality risk in NHANES(2015–2018); (O)ROC curve of hs-CRP for cardiovascular mortality risk in NHANES(2015–2018); (P)ROC curve of hs-CRP/Albumin for cardiovascular mortality risk in NHANES(2015–2018).
Annotation: The images enclosed in red boxes represent the ROC curves for all-cause mortality risk for each study period (2007–2010, 2015–2018), while the remaining plots represent the ROC curves for cardiovascular mortality risk.
Mediation analysis
Correlation analysis revealed that higher LE8 were significantly associated with lower levels of inflammatory and insulin resistance indices across all models (Supplementary Table 4). Specifically, in Model 3, LE8 was negatively associated with Ln(SII) (Beta = −0.05; 95% CI: −0.06, −0.04; P < 0.001) and Ln(SIRI) (Beta = −0.05; 95% CI: −0.06, −0.04; P < 0.001). Similarly, LE8 demonstrated an inverse relationship with HOMA-IR (Beta = −0.67; 95% CI: −0.83, −0.52; P < 0.001). In terms of traditional inflammatory markers, LE8 was negatively correlated with CRP (Beta = −0.09; 95% CI: −0.12, −0.07; P < 0.001) and the CRP/Albumin ratio (Beta = −0.02; 95% CI: −0.03, −0.02; P < 0.001). For hs-CRP and the hs-CRP/Albumin ratio, significant negative associations were also observed (Beta = −0.74; 95% CI: −1.00, −0.45; P < 0.001 and Beta = −0.20; 95% CI: −0.28, −0.13; P < 0.001, respectively). However, LE8 was not significantly associated with ferritin in Model 3.
Supplementary Table 5 demonstrates the mediation effects of inflammatory and insulin resistance markers in the relationship between LE8 and MAFLD. Among these markers, the HOMA-IR index exhibited the highest mediation effect, accounting for 72.26% (95% CI: 63.25%, 78.33%). For inflammatory markers, CRP and CRP/Albumin ratio mediated 10.84% (95% CI: 6.63%, 17.26%) and 10.86% (95% CI: 6.37%, 17.06%), respectively. hs-CRP and hs-CRP/Albumin ratio mediated 10.67% (95% CI: 5.81%, 18.71%) and 11.37% (95% CI: 6.16%, 19.25%). Ln(SIRI) and Ln(SII) also showed significant mediation effects, accounting for 3.04% (95% CI: 1.87%, 4.58%) and 3.66% (95% CI: 2.40%, 5.26%), respectively.
Supplementary Tables 6 and 7 present the mediation effects of these markers on the relationship between LE8 and mortality. For all-cause mortality(Supplementary Table 6), significant mediation effects were observed for Ln(SIRI) (11.18%, 95% CI: 6.75%, 18.85%), Ln(SII) (5.86%, 95% CI: 1.90%, 11.16%), CRP (11.14%, 95% CI: 3.23%, 29.29%), and CRP/Albumin ratio (11.29%, 95% CI: 4.99%, 34.44%). For cardiovascular mortality, Supplementary Table 7 highlights that Ln(SIRI) (16.74%, 95% CI: 7.70%, 52.60%; P = 0.004) and Ln(SII) (14.69%, 95% CI: 6.38%, 61.22%; P = 0.012) were significant mediators. CRP, hs-CRP, CRP/Albumin ratio, and hs-CRP/Albumin did not demonstrate significant mediation effects. However, no mediation effects were observed for HOMA-IR and ferritin in the relationship between LE8 and mortality risk.
Subgroup analyses and interaction tests
The results of the subgroup analyses are shown in Fig. 7. LE8 were negatively associated with MAFLD across all subgroups (Fig. 7A). This negative association remained consistent after stratifying by sex, age, race, marital status, education, PIR, and hypertension. Notably, a significant interaction was observed between LE8, age, and hypertension (P < 0.05 for interaction) in the relationship with MAFLD, indicating that the protective effect of LE8 against MAFLD was stronger in individuals without hypertension and those aged 20–60 years.
In the analysis of all-cause mortality (Fig. 7B), a significant interaction between LE8 and age was identified, with the association between LE8 and reduced mortality risk being stronger in the 20–60 age group compared to the 60–80 age group. Regarding cardiovascular mortality (Fig. 7B), significant interactions were observed between LE8, age, and race (P < 0.05), indicating that the protective effect of LE8 against cardiovascular mortality was more pronounced in younger individuals and varied across different racial groups.
Discussion
High LE8 scores were found to significantly reduce the prevalence of MAFLD in overweight and obese populations, with insulin resistance and inflammation playing a mediating role. Additionally, LE8 was associated with reduced mortality risk through the improvement of inflammation. Kaplan-Meier curves revealed significantly lower survival rates in the group with low LE8 levels. RCS curves showed a non-linear relationship between LE8 and MAFLD, with benefits increasing as LE8 scores rise. The novel inflammatory marker SIRI demonstrated its potential as a robust predictor of mortality risk in overweight and obese populations in ROC analysis. Furthermore, interaction tests revealed a significant interaction between LE8 and age across all subgroups analysis, indicating that individuals in the 20–60 age group are more likely to benefit from higher LE8 scores compared to those in the 60–80 age group.
To the best of our knowledge, LE7, the predecessor of LE8, has been repeatedly shown to be negatively associated with NAFLD43,44. Regarding LE8, several studies have explored its relationship with NAFLD and mortality. He et al. used data from the UK Biobank, including 266,645 participants, and found that higher LE8 scores, reflecting a better lifestyle, significantly reduced the prevalence of NAFLD. Over a median follow-up of 11.9 years, the high LE8 group had a 90% lower risk of NAFLD compared to the low LE8 group45. A study using a single NHANES cycle also demonstrated a negative association between LE8 and NAFLD, with the high LE8 group showing a 33% reduced risk of NAFLD compared to the low group25. MAFLD encompasses a broader range of fatty liver diseases, yet studies investigating the relationship between LE8 and MAFLD in overweight and obese populations are limited.
Our results also confirm previous studies. Meanwhile, as we concerned, the exclusive definition of NAFLD excludes certain fatty liver disease patients from many studies. Specifically, the threshold for alcohol consumption in alcoholic fatty liver disease varies across different guidelines46. Additionally, there is considerable heterogeneity in how individuals metabolize alcohol. Several studies have indicated that, while there is some difference in the prevalence of MAFLD and NAFLD in the general population, the difference is not substantial47,48. However, for overweight/obese individuals, the definition of MAFLD is more advantageous for managing fatty liver disease42. In our study, 3,233 participants (weighted 46%) were diagnosed with MAFLD, while 1,458 participants (weighted 18%) were diagnosed with NAFLD. Our study found that the risk of MAFLD decreased by 89% in the high LE8 group compared to the low LE8 group, and this population is more likely to benefit from LE8. Additionally, a study showed that the high LE8 group had a 40% reduction in all-cause mortality and a 54% reduction in cardiovascular mortality compared to the low LE8 group11. In our study, all-cause mortality and cardiovascular mortality were reduced by 58% and 90%, respectively. These findings provide valuable insights for future health management strategies for the obese population.
Inflammation and insulin resistance play central roles in the initiation and progression of MAFLD5. Furthermore, in overweight and obese populations, levels of several inflammatory markers, such as C-reactive protein (CRP), interleukin-6 (IL-6), and tumor necrosis factor-alpha (TNF-α), are elevated compared to normal levels49,50,51. These metabolic and immune responses often overlap in individuals, suggesting that they are frequently in a state of chronic low-grade inflammation or mild metabolic disorders52. This contributes, in part, to their increased risk of immune-related diseases and cardiovascular events21. In our study, insulin resistance indices, along with various inflammatory markers, were positively correlated with the prevalence of MAFLD. A significant portion of LE8’s positive impact on MAFLD was mediated through the improvement of insulin resistance, with HOMA-IR accounting for 72.26% of the mediation effect. Improvements in inflammation, including CRP, CRP/Albumin, SII, and SIRI indices, also contributed to the observed effects, with mediation effects ranging from 3 to 12%. It is worth noting that SII and SIRI are novel systemic immune and inflammatory indices13. These indices may be influenced by regulatory actions from multiple organs in the body. Such factors could, in turn, affect the mediation statistics. Furthermore, LE8 also reduces mortality risk through its effects on inflammation.
MAFLD and NAFLD share a highly overlapping pathological mechanism. In addition to the potential involvement of inflammatory factors and insulin resistance, several other mechanisms may contribute to the pathogenesis of MAFLD. A key mechanism is the dysregulation of adipokines53. In obesity, an imbalance in the secretion of adipokines, including leptin, adiponectin, and resistin, has been observed. Leptin, which is typically elevated in obesity, promotes liver inflammation and fibrosis. In contrast, adiponectin, which exerts anti-inflammatory and insulin-sensitizing effects, is usually decreased in obese individuals, thereby exacerbating hepatic steatosis and inflammation54. Additionally, hepatic mitochondrial dysfunction has been implicated in disease development. Obesity-induced oxidative stress leads to mitochondrial damage, impairing the liver’s ability to efficiently oxidize fatty acids, thereby contributing to disease progression55.
The present study has several strengths. To our knowledge, it is the first to assess the role of inflammation and insulin resistance in mediating the relationship between LE8 and MAFLD as well as mortality. Additionally, we included participant data from six cycles, which enhances the generalizability of the findings to a broader population. However, there are some limitations. Due to the design of the NHANES database, data for CRP and hs-CRP were partially missing. This limitation, coupled with the relatively small sample size, may introduce bias into some of the results, and larger studies are needed to confirm these findings. As a retrospective study, we can only draw associations, and further cohort studies are required to establish causality. Furthermore, lifestyle factors such as diet, physical activity, smoking, and sleep were collected via self-reported questionnaires, which may introduce measurement bias. Finally, due to the lack of a gold standard for diagnosing hepatic steatosis in the included data, we used the US-FLI index, which may have introduced some diagnostic bias.
Conclusion
In this nationally representative sample, higher LE8 scores were associated with a lower prevalence of MAFLD and a reduced risk of mortality in overweight and obese populations, potentially mediated through improvements in inflammation and insulin resistance. These findings highlight the importance of primary prevention strategies aimed at maintaining optimal cardiovascular health, which can significantly reduce both the prevalence of MAFLD and the risk of mortality, particularly in overweight and obese individuals.
Data availability
The datasets ANALYZED for this study can be found in the NHANES(https://www.cdc.gov/nchs/nhanes/index.htm).
References
Riazi, K. et al. The prevalence and incidence of NAFLD worldwide: a systematic review and meta-analysis. Lancet Gastroenterol. Hepatol. 7, 851–861 (2022).
Quek, J. et al. Global prevalence of non-alcoholic fatty liver disease and non-alcoholic steatohepatitis in the overweight and obese population: a systematic review and meta-analysis. Lancet Gastroenterol. Hepatol. 8, 20–30 (2023).
Chalasani, N. et al. The diagnosis and management of nonalcoholic fatty liver disease: practice guidance from the American association for the study of liver diseases. Hepatology 67, 328–357 (2018).
Eslam, M., Sanyal, A. J., George, J. & International Consensus Panel MAFLD: A Consensus-Driven proposed nomenclature for metabolic associated fatty liver disease. Gastroenterology 158, 1999–2014 (2020). .e1.
Friedman, S. L., Neuschwander-Tetri, B. A., Rinella, M. & Sanyal, A. J. Mechanisms of NAFLD development and therapeutic strategies. Nat. Med. 24, 908–922 (2018).
Haukeland, J. W. et al. Systemic inflammation in nonalcoholic fatty liver disease is characterized by elevated levels of CCL2. J. Hepatol. 44, 1167–1174 (2006).
Lomonaco, R. et al. Effect of adipose tissue insulin resistance on metabolic parameters and liver histology in obese patients with nonalcoholic fatty liver disease. Hepatology 55, 1389–1397 (2012).
Lloyd-Jones, D. M. et al. Life’s essential 8: updating and enhancing the American heart association’s construct of cardiovascular health: A presidential advisory from the American heart association. Circulation 146, e18–43 (2022).
Lloyd-Jones, D. M. et al. Defining and setting National goals for cardiovascular health promotion and disease reduction: the American heart association’s strategic impact goal through 2020 and beyond. Circulation 121, 586–613 (2010).
Lloyd-Jones, D. M. et al. Status of cardiovascular health in US adults and children using the American heart association’s new life’s essential 8 metrics: prevalence estimates from the National health and nutrition examination survey (NHANES), 2013 through 2018. Circulation 146, 822–835 (2022).
Yi, J., Wang, L., Guo, X. & Ren, X. Association of life’s essential 8 with all-cause and cardiovascular mortality among US adults: A prospective cohort study from the NHANES 2005–2014. Nutr. Metab. Cardiovasc. Dis. 33, 1134–1143 (2023).
Mirjalili, S. R. et al. An innovative model for predicting coronary heart disease using triglyceride-glucose index: a machine learning-based cohort study. Cardiovasc. Diabetol. 22, 200 (2023).
Ma, G. et al. Systemic inflammation mediates the association between environmental tobacco smoke and depressive symptoms: A cross-sectional study of NHANES 2009–2018. J. Affect. Disord. 348, 152–159 (2024).
Guo, B. et al. Associations of CBC-Derived inflammatory indicators with sarcopenia and mortality in adults: evidence from Nhanes 1999 ∼ 2006. BMC Geriatr. 24, 432 (2024).
Zhou, Z. et al. Neutrophil–Hepatic stellate cell interactions promote fibrosis in experimental steatohepatitis. Cell. Mol. Gastroenterol. Hepatol. 5, 399–413 (2018).
Tilg, H., Adolph, T. E., Dudek, M. & Knolle, P. Non-alcoholic fatty liver disease: the interplay between metabolism, microbes and immunity. Nat. Metab. 3, 1596–1607 (2021).
Miele, L. et al. Nonalcoholic fatty liver disease (NAFLD) severity is associated to a nonhemostatic contribution and Proinflammatory phenotype of platelets. Transl Res. 231, 24–38 (2021).
Liu, K. et al. Systemic immune-inflammatory biomarkers (SII, NLR, PLR and LMR) linked to non-alcoholic fatty liver disease risk. Front. Immunol. 15, 1337241 (2024).
Zhao, E., Cheng, Y., Yu, C., Li, H. & Fan, X. The systemic immune-inflammation index was non-linear associated with all-cause mortality in individuals with nonalcoholic fatty liver disease. Ann. Med. 55:2197652 .
Liu, Q. et al. Shift in prevalence and systemic inflammation levels from NAFLD to MAFLD: a population-based cross-sectional study. Lipids Health Dis. 22, 185 (2023).
Gregor, M. F. & Hotamisligil, G. S. Inflammatory mechanisms in obesity. Annu. Rev. Immunol. 29, 415–445 (2011).
NHANES - National Health and Nutrition Examination Survey Homepage. Aug (2024). https://www.cdc.gov/nchs/nhanes/index.htm. Accessed 5.
Xu, W. et al. Association between the AHA life’s essential 8 and prediabetes/diabetes: a cross-sectional NHANES study. Front. Endocrinol. ;15. (2024).
Huang, W. et al. Association between life’s essential 8 and male biochemical androgen deficiency: evidence from NHANES 2013–2016. Front. Endocrinol. (Lausanne). 15, 1369684 (2024).
Wang, L., Yi, J., Guo, X. & Ren, X. Associations between life’s essential 8 and non-alcoholic fatty liver disease among US adults. J. Transl Med. 20, 616 (2022).
Krebs-Smith, S. M. et al. Update of the healthy eating index: HEI-2015. J. Acad. Nutr. Diet. 118, 1591–1602 (2018).
Tian, T. et al. Dietary quality and relationships with metabolic Dysfunction-Associated fatty liver disease (MAFLD) among united States adults, results from NHANES 2017–2018. Nutrients 14, 4505 (2022).
Yuguang, L. et al. Inflammation mediates the relationship between diet quality assessed by healthy eating index-2015 and metabolic syndrome. Front. Endocrinol. (Lausanne). 15, 1293850 (2024).
Questionnaires, N. H. A. N. E. S. & Documentation, R. Datasets, and Aug. (2024). https://wwwn.cdc.gov/nchs/nhanes/Default.aspx. Accessed 5.
Pan, J., Zhou, Y., Pang, N. & Yang, L. Dietary niacin intake and mortality among individuals with nonalcoholic fatty liver disease. JAMA Netw. Open. 7, e2354277 (2024).
Eslam, M. et al. A new definition for metabolic dysfunction-associated fatty liver disease: an international expert consensus statement. J. Hepatol. 73, 202–209 (2020).
What Is, A. & Standard Drink? | National Institute on Alcohol Abuse and Alcoholism (NIAAA). Aug. (2024). https://www.niaaa.nih.gov/alcohols-effects-health/overview-alcohol-consumption/what-standard-drink. Accessed 5.
Ruhl, C. E. & Everhart, J. E. Fatty liver indices in the multiethnic united States National health and nutrition examination survey. Aliment. Pharmacol. Ther. 41, 65–76 (2015).
NCHS Data Linkage - Mortality Data. (2024). https://www.cdc.gov/nchs/data-linkage/mortality.htm. Accessed 5 Aug 2024.
Wang, D. et al. Terpene mixtures and metabolic syndrome in the US general population: exploring the mediating role of insulin resistance. BMC Public. Health. 24, 3587 (2024).
Yuan, M. et al. Hypertension and NAFLD risk: insights from the NHANES 2017–2018 and Mendelian randomization analyses. Chin. Med. J. (Engl). 137, 457–464 (2024).
Jiang, Q., Jiang, Y., Ma, Z., Huang, J. & Li, Y. Nonlinear correlation and mediation effects between serum 25-hydroxyvitamin D levels and all-cause mortality in COPD patients. Front. Nutr. 11, 1412606 (2024).
Huang, Q. et al. Association between manganese exposure in heavy metals mixtures and the prevalence of sarcopenia in US adults from NHANES 2011–2018. J. Hazard. Mater. 464, 133005 (2024).
Du, W. et al. Association between dietary magnesium intake and gallstones: the mediating role of atherogenic index of plasma. Lipids Health Dis. 23, 82 (2024).
Xu, B. et al. Is systemic inflammation a missing link between cardiometabolic index with mortality? Evidence from a large population-based study. Cardiovasc. Diabetol. 23, 212 (2024).
Guo, J. et al. Environmental toxicant exposure and depressive symptoms. JAMA Netw. Open. 7, e2420259 (2024).
Liu, J. et al. Estimating global prevalence of metabolic Dysfunction-Associated fatty liver disease in overweight or obese adults. Clin. Gastroenterol. Hepatol. 20, e573–e582 (2022).
Liu, H. et al. Ideal cardiovascular health metrics and the risk of non-alcoholic fatty liver disease: A cross-sectional study in Northern China. Liver Int. 39, 950–955 (2019).
Jang, E-H. et al. Cardiovascular health metrics in the development and regression of nonalcoholic fatty liver disease: A cohort study. J. Clin. Med. 8, 610 (2019).
He, P. et al. A healthy lifestyle, life’s essential 8 scores and new-onset severe NAFLD: A prospective analysis in UK biobank. Metabolism 146, 155643 (2023).
European Association for the Study of the Liver (EASL). European association for the study of diabetes (EASD), European association for the study of obesity (EASO). EASL-EASD-EASO clinical practice guidelines for the management of non-alcoholic fatty liver disease. J. Hepatol. 64, 1388–1402 (2016).
Song, R., Li, Z., Zhang, Y., Tan, J. & Chen, Z. Comparison of NAFLD, MAFLD and MASLD characteristics and mortality outcomes in united States adults. Liver Int. 44, 1051–1060 (2024).
Vaz, K. et al. Current Understanding and future perspectives on the impact of changing NAFLD to MAFLD on global epidemiology and clinical outcomes. Hepatol. Int. 17, 1082–1097 (2023).
Hebib, L. et al. Life’s essential 8 is inversely associated with high-sensitivity C-reactive protein. Sci. Rep. 14, 15024 (2024).
Saltiel, A. R. & Olefsky, J. M. Inflammatory mechanisms linking obesity and metabolic disease. J. Clin. Invest. 127, 1–4 (2017).
Li, L. & Dai, F. Comparison of the associations between life’s essential 8 and life’s simple 7 with depression, as well as the mediating role of oxidative stress factors and inflammation: NHANES 2005–2018. J. Affect. Disord. 351, 31–39 (2024).
Hotamisligil, G. S. Inflammation and metabolic disorders. Nature 444, 860–867 (2006).
Powell, E. E., Wong, V. W. S. & Rinella, M. Non-alcoholic fatty liver disease. Lancet 397, 2212–2224 (2021).
Ahima, R. S. & Lazar, M. A. Physiology. The health risk of obesity–better metrics imperative. Science 341, 856–858 (2013).
Sanyal, A. J. et al. Nonalcoholic steatohepatitis: association of insulin resistance and mitochondrial abnormalities. Gastroenterology 120, 1183–1192 (2001).
Acknowledgements
Thanks to all who contributed to the NHANES study.
Funding
This work was supported by the Hunan Provincial Natural Science Foundation Science and Health Joint Project Grant Number[2023 JJ60044]; Hunan Province Traditional Chinese Medicine Research Program Project Grant Number[B2023079]; Hunan Province Clinical Medical Technology Innovation Guidance Project Grant Number[2021SK51413]; Excellent Youth Project of the Research Program of Hunan Provincial Department of Education Grant Number[21B0389]; Scientific Research Project of Education Department of Hunan Province[24 A0274]; and the Domestic First-class Construction Discipline of Chinese Medicine in Hunan University of Chinese Medicine.
Author information
Authors and Affiliations
Contributions
ZWJ and XY were responsible for the study conception and study design. LJY and ZDX were involved in data acquisition and study execution.ZM, FH, TCS and XJ analyzed the data and drafted the manuscript. ZQ, YWQ and TXQ conducted repeatability analysis on the data. ZML contributed to interpretation and editing of the manuscript. All authors agree to be accountable for the content of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Ethics statement
Ethical approval for NHANES was secured from the NCHS Research Ethics Review Board, and each participant willingly provided written informed consent.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhang, W., Zou, M., Liang, J. et al. Association of cardiovascular health with MAFLD and mortality in overweight and obese adults and mediation by inflammation and insulin resistance. Sci Rep 15, 18791 (2025). https://doi.org/10.1038/s41598-025-03820-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-03820-z