SUMMARY
Chemotherapy-induced peripheral neuropathy (CIPN) is a debilitating and painful condition seen in patients undergoing treatment with common agents such as vincristine, paclitaxel, oxaliplatin and bortezomib. The mechanisms of this condition are diverse, and include an array of molecular and cellular contributions. Current research implicates genetic predispositions to this condition, which then may influence cellular responses to chemotherapy. Processes found to be influenced during CIPN include increased expression of inflammatory mediators, primarily cytokines, which can create cascading effects in neurons and glia. Changes in ion channels and neurotransmission, as well as changes in intracellular signaling and structures have been implicated in CIPN. This review explores these issues and suggests considerations for future research.
Keywords: chemotherapy, cytokine, glial cells, ion channels, neuropathy, neurotransmission
Chemotherapy-induced peripheral neuropathy (CIPN) is a frequent side effect for many of the most common cancer treatments and is characterized by paresthesia, dysesthesia and often pain, primarily in the hands and feet. Patients most often report sensory symptoms of numbness and tingling, followed by symptoms described as burning, shooting, throbbing and stabbing. All of these symptoms are also associated with diminished ability to detect touch and pinprick sensations as well as sensorimotor impairment [1]. These sensory changes can be debilitating to the extent that a reduction in the dose of therapy given to a patient is required. For example, a recent report found that 17% of patients receiving the chemotherapeutic agent paclitaxel required a dose reduction because of CIPN, and such dose reductions have been linked to poorer survival rates [2].
The occurrence of CIPN has been studied for decades and is commonly associated with well-known anticancer drugs. Those therapies most likely to produce CIPN include cisplatin [3] oxaliplatin [4,5], vincristine [6,7], paclitaxel [8] and bortezomib [1]. Each of these agents works to kill cancerous cells in differing ways and produces various rates of CIPN. To illustrate, approximately 40% of patients receiving cisplatin or paclitaxel will experience CIPN, whereas an estimated 80% of patients undergoing treatment with oxaliplatin will report extreme sensitivity to cold [9]. The occurrence of CIPN is generally related to dosing, both in the amount of drug administered and in the number of administrations, and to various risk factors such as diabetes or a history of smoking.
Unfortunately, these symptoms may persist beyond treatment. One report demonstrated that CIPN following paclitaxel or vincristine administration lasting longer than 3 months became chronic. For this cohort of patients, the average time with neuropathy was 5 years, and their pain was poorly managed by current treatments, including opiates [10]. As would be expected, these symptoms significantly reduce quality of life [11]. These factors bolster the need to better understand the mechanisms driving the development of CIPN.
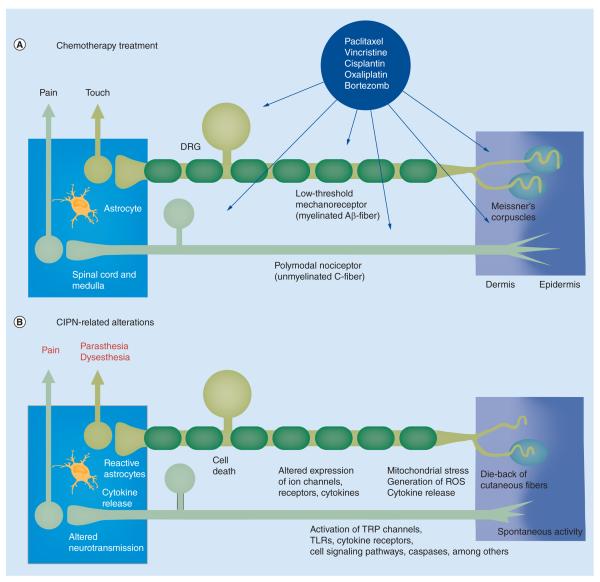
Chemotherapy treatments result in numerous changes to cellular structure and function, including loss of sensory terminals in the skin, and alterations of membrane receptors, intracellular signaling, neurotransmission, excitability and metabolism all of which can negatively influence neuronal and glial cell phenotypes, thereby contributing to CIPN (Figure 1). This complexity has hindered a unified understanding of the specific mechanisms underlying this condition. As a step toward formulating a unifying hypothesis, the scope of this review is to inform the reader of the major biological factors involved in effects of chemotherapy on the nervous system that contribute to CIPN.
Figure 1. Schematic overview of mechanisms of chemotherapy-induced peripheral neuropathy.
(A) Illustrates neuronal and glial targets for chemotherapeutics, including paclitaxel, bortezomib and oxaliplatin. (B) Indicates the mulitple ways these drugs alter neuron and glial cell function, resulting in activation of astrocytes, enhanced cytokine release, mitotoxicity and eventual apoptosis, spontaneous discharge and altered signaling in primary afferent fibers, and loss of cutaneous fibers, ultimately enhancing nociceptive input.
CIPN: Chemotherapy-induced peripheral neuropathy; DRG: Dorsal root ganglion; ROS: Reactive oxygen species; TLR: Toll-like receptor; TRP: Transient receptor potential.
Genetic influences
With the growing trend of personalized medicine, recent studies have turned toward understanding CIPN from a pharmacogenomic perspective. This approach would potentially allow practitioners to identify patients who carry genetic variations that would increase their risk of chemotherapy-related side effects such as CIPN and modify treatment as necessary. Multiple studies, with each generally focusing on one type of cancer and treatment, have investigated the relationship between single nucleotide polymorphisms (SNPs) and CIPN risk. A concise review of the genes and SNPs that have been implicated as potentially predictive for CIPN was recently published [12]. Unfortunately, the results from these studies have not always been reproducible. For example, many studies have investigated the GSTP1 gene. Earlier reports found that polymorphisms in this gene were related to survival outcomes in cancer [13] making it a viable candidate for pharmacogenomics research. While some have indeed found an association between GSTP1 polymorphisms and CIPN [14], just as many have failed to find a relationship (c.f. [15]), even when controlling for ethnicity, type of cancer and primary treatment. That being said, this line of investigation warrants more research because most studies have focused on genes involved in cancer rather than on genes likely to contribute more specifically to neuropathy. Some recent studies have shown predictive validity when studying the contribution of SNPs to CIPN. For example, patients undergoing treatment with oxaliplatin had five SNPs identified that predicted CIPN development with 72% accuracy [16]. Others extended these predictive findings to additional polymorphisms found in Charcot-Marie-Tooth disease genes [17]. The genes that were found to be significantly associated with CIPN were related to myelinating Schwann cells (periaxin), nerve conduction velocity (Rho guanine nucleotide exchange factor 10) and tachykinin peptide production (tachykinin precursor 1). This line of research is promising, but future studies will need to elucidate how these mutations influence CIPN development. This is especially important in light of research demonstrating that survival rates are reduced by treatment modifications.
Neuronal alterations associated with CIPN
Much of the research on the mechanisms of CIPN has focused on alterations produced by chemotherapy drugs on neuronal properties, including altered ion channel responses and activation or modification of intracellular signaling pathways.
• Altered activity & expression of voltage-gated ion channels in CIPN
As Na+ entry into a neuron is usually the primary cause of excitation and depolarization, it is not surprising that changes in the behavior of voltage-gated sodium channels have been found in CIPN. For example, a major metabolite of oxaliplatin, oxalate, can produce prolonged opening of voltage-gated Na+ channels, leading to altered thresholds and ectopic firing in diverse neurons [18,19]. Consistent with the possibility of enhanced activity in sodium channels (or depressed activity in potassium channels) increased peripheral axonal excitability precedes symptom expression in patients [20,21]. Interestingly, voltage-gated sodium channel blockers, such as the anticonvulsant carbamazepine, have shown some success in treating neuropathy in people [22], although not all clinical studies have supported the effectiveness of this approach [23].
Potassium channel changes in CIPN have been proposed at various levels of the nervous system. Cortical level K+ channels were down-regulated in rats treated with oxaliplatin, an effect the authors proposed contributes to the ongoing nature of CIPN [24]. Primary afferent fibers also exhibit decreased expression of various potassium channels in both oxaliplatin [25] and paclitaxel models of CIPN [26]. These changes result in a more depolarized resting membrane potential, leading to hyperexcitability in nociceptors and could be related to the development of spontaneous activity in DRG neurons in CIPN rats [26]. Interestingly, both of these studies also found increased expression of hyperpolarization-activated channels (HCNs) permeable to both K+ and Na+, which are known to increase nociceptor excitability and spontaneous firing in other pain conditions [27]. A simulation study has shown that oxaliplatin-induced decreases in potassium channel function and increases in sodium channel function can account for the observed nociceptor hyperexcitability [28]. In support of these findings, use of a voltage-gated K+ channel opener, retigabine, to encourage neuronal hyperpolarization has been found to be effective in a mouse model of cisplatin neuropathy [29].
Calcium is an important contributor to CIPN in numerous ways. Voltage-gated calcium channels are essential for nociceptive signal transmission, and appear to contribute to CIPN as well. Increased levels of voltage-gated calcium channel mRNA have been reported in DRG following paclitaxel treatment in mice [30], and administration of drugs that interfere with the function of voltage-gated calcium channels, such as gabapentin and ethosuximide, reduced paclitaxel- and vincristine-induced reflex hypersensitivity in rodents [31,32].
• Alterations of neurotransmission in CIPN
Numerous studies have documented alterations in processes involved primarily in neurotransmitter signaling following chemotherapy treatment. 5HT2A knockout mice failed to develop vincristine-induced mechanical hyperalgesia, and rats exposed to vincristine had increased expression of this receptor in the spinal cord [33]. Similar results have been obtained for vincristine-induced neuropathy in mice lacking serotonin transporters [34].
Glutamate signaling is also altered in CIPN. Pharmacological inhibition of glutamate production by blocking the enzyme glutamate decarboxypeptidase (which hydrolyzes the peptide N-acetyl-aspartyl-glutamate to release glutamate) improved nerve conduction deficits and reversed morphological alterations in DRGs associated with CIPN following cisplatin, paclitaxel and bortezomib [35]. Administration of an mGluR5 antagonist reversed bortezomib-induced reflex hypersensitivity and nerve conduction deficits [36]. Furthermore, as glutamate is an excitatory neurotransmitter, its clearance from the synapse prevents excitotoxicity, and reduced clearance by astrocytes can lead to increased responses of spinal neurons to nociceptive input [37]. Bortezomib-, paclitaxel- and vincristine-induced hyperalgesia in the rat have all been associated with decreased expression of the glutamate transporter GLAST in spinal astrocytes [38,39]. Given that spinal neurons show pronounced after discharges that appear to be related to the downregulation of glutamate transporters and that similar changes in spinal neuron physiology are observed in vincristine – and cisplatin-induced neuropathies [40,41], downregulation of glutamate transporters may be a common mechanism across CIPN subtypes.
Changes to other neurotransmitter systems have been also observed in animal models of CIPN, including decreased spinal mu-opioid receptor activation by the endogenous ligand, endomorphin-1 [42]. It was proposed that the resulting effect is due to an indirect loss of inhibitory GABA signaling that could be differentially reversed by oxycodone, but not morphine [35]. Unfortunately, clinical use of an array of opiate analgesics does not adequately treat CIPN [10]. Altering levels of endocannabinoids may prove useful in CIPN treatment. Endocannabinoids are broken down by fatty acid amide hydrolase (FAAH), and blocking this enzyme to increase endocannabinoid levels can reverse cold and mechanical sensitivity [43] and decrease C-fiber sensitization in a cisplatin model of CIPN [44]. Recently, translational research aimed at augmentation of signaling by A3 adenosine receptors has been suggested as an effective treatment for paclitaxel-related CIPN [45].
• Alterations of transient receptor potential channels in CIPN
The transient receptor potential (TRP) channels are a large family of nonselective cation channels. The TRP vanilloid (TRPV) family has been the most widely studied with regard to pain. TRPV1, the capsaicin receptor, is located on a large subset of nociceptors and plays important roles in sensory transduction and primary afferent sensitization. This channel can be activated in numerous ways, including by various exogenous vanilloid chemicals (e.g., capsaicin, resiniferatoxin) as well as by protons, heat greater than 42°C, and diverse endogenous lipid signals associated with inflammation [46]. Predictably, the sensation evoked by these stimuli when applied to skin is perceived by humans as a burning sensation [47]; but surprisingly is perceived as deep aching pain following intramuscular administration [48,49]. Notably, CIPN patients complain of both these symptoms [1,10]. Indeed, recent evidence indicates that activation of TRPV1 during chemotherapy sensitizes pain pathways. The expression of TRPV1 is increased in rat DRG following paclitaxel administration at a time point corresponding to the onset of thermal hyperalgesia; and use of TRPV1 antagonists in a rodent model reduced heat hypersensitivity [50]. Increases in TRPV1 expression in murine DRG and spinal cord have also been observed following bortezomib [51] and cisplatin treatments [52].
TRPA1 is often colocalized with TRPV1 and can be activated by diverse noxious chemicals including formalin, allyl isothiocyanate and acrolein; and by cold temperatures (≤17°C) under some conditions [53]. Oxaliplatin produces a robust sensitivity to cold in most patients, and based on animal studies indicating that TRPA1 channels respond to noxious cold [54], it was assumed that this channel was responsible for this effect. Indeed, studies reported that oxaliplatin-induced sensitivity to cold in animal models was TRPA1 dependent [55,56]. This conclusion was also drawn for paclitaxel-induced cold allodynia [57]. However, recent research has proposed a species-dependent activation of this channel, wherein noxious cold activates TRPA1 in rodents but not humans [58], thereby limiting the potential translational impact of TRPA1 channels as cold sensors. Yet, the possibility remains that TRPA1 may be involved in the induction of long-lasting sensitization of nociceptors during chemotherapy. Ongoing CIPN may be supported by sensitization of TRPV1, TRPV4 and TRPA1 channels by enzymes (protein kinase A, protein kinase C epsilon, phospholipase C) activated by proteinase-activated receptors (PARs) after chemotherapy [59].
Finally, less studied, but also a potentially important modulator of CIPN is the TRPM8 channel. The TRPM8 channel is activated by mild cool stimuli between 25 and 28°C and chemically by menthol [60] and has been implicated as analgesic when activated in some nerve injury models [61]. An analgesic effect of topical menthol has also been reported in paclitaxel-related CIPN patients [62].
• Intracellular signaling pathways associated with CIPN
Activation of protein kinases and caspases occurs during various forms of cellular stress and in response to growth factors and cytokines. Activation of these enzymes can result in mitochondrial damage and apoptosis in neurons and glial cells.
Caspase signaling is thought to contribute to CIPN via its relation to mitochondrial damage and observed DRG cell loss. Animal models indicate that paclitaxel activates the caspase 10 pathway, leading to mitochondrial damage and subsequently to the generation of reactive oxygen species (ROS), as well as potential apoptosis of the neuron [63]. Caspase signaling was also found to contribute to cisplatin and oxaliplatin neuropathy in rats, with activation of these pathways caused by mitochondrial ROS production [64]. Caspase inhibitors reduce vincristine-induced reflex hypersensitivity in the rat [65] and prevent oxaliplatin-induced DRG cell loss [66].
Activation of protein kinase pathways, especially kinases in the MAPK family, can further contribute to cellular damage. Cisplatin and oxaliplatin activate p38 MAPK and Erk1/2 to promote apoptosis in DRG neurons [67]. A follow up study by this group replicated kinase activation changes and further reported a protection against this apoptosis by NGF [68]. Activation of these pathways influence a number of downstream events that could further promote CIPN, including cytokine release and damage to cellular structures.
Changes to intracellular structures associated with CIPN
Damage to glial and neuronal mitochondria as a result of chemotherapy has been the focus of much of the recent research on CIPN. Some rodent studies have reported swollen and vacuolated mitochondria and or impaired mitochondrial function following treatment with paclitaxel [69–71], oxaliplatin [71,72] and bortezomib [73]. Acetyl l-carnitine (ALCAR) has been reported to improve mitochondrial function following chemotherapy and became a promising avenue of CIPN therapy, with several studies in animal models reporting resolution of chemotherapy-induced mechanical and thermal hyperalgesia [74–77]. Initial clinical trials showed promise with ALCAR [78,79] but, unfortunately, subsequent trials found that ALCAR not only fails to have a significant ameliorating effect [80], but can actually worsen CIPN [81]. Thus, it remains unclear whether the clinical trial results negate the hypothesis of a central role of mitotoxicity in the pathophysiology of CIPN.
Oxidative stress is both a catalyst for and a product of mitochondrial distress. Bortezomib can induce reactive oxygen species (ROS) to produce mitochondrial dysfunction [82]. Paclitaxel can also increase mitochondrial production of ROS, which can sensitize TRPA1 channels to enhance thermal sensitivity in rodents [83]. As mentioned previously, mitochondrial-released ROS can then activate apoptotic and proinflammatory pathways, contributing to chronic CIPN. Further evidence for a role of ROS in CIPN was the finding that administration of ROS scavengers alleviates paclitaxel-induced mechanical hyperalgesia [84,85]. Peroxynitrite, a powerful oxidant and nitrating agent produced by ROS, has been proposed as a potential therapeutic target for ameliorating CIPN based on translational work in rodents [86].
Damage to DNA, due to direct effects of chemotherapeutics on neurons as well as ROS production during mitochondrial distress, has been strongly implicated in CIPN [87]. Cisplatin and oxaliplatin produce DNA adducts, leading to neuron death [62]. Apurinic/apyrimidinic endonuclease/redox effector factor (APE1), an ezyme which contributes to DNA repair, has been implicated as a potential therapeutic target for CIPN. Decreased expression of APE1 is associated with increased nociceptive responding following cisplatin and oxaliplatin, and enhancing the activity of this enzyme protected against cisplatin-induced neurotoxicity of cultured neurons [88].
Other cellular components can be damaged in CIPN. Bortezomib and cisplatin can damage organelles, such as lysosomes and endoplasmic reticulum in neurons [89,90] and Schwann cells [91]. Many of the common chemotherapeutics target microtubules in cancer cells to prevent cellular division, and binding of these drugs to neuronal microtublues has been suggested as contributing to CIPN [92–94]. Axonal transport in peripheral nerves is in fact impaired following treatment with vincristine and paclitaxel [94,95]. However, neither oxaliplatin nor bortezomib bind to microtubules when used to produce cancer cell death, yet both still produce a robust neuropathy in a clinical population [1,92]. Interestingly, both bortezomib and oxaliplatin inhibit axonal transport like the antimicrotubule agents [96,97]. Suppression of axonal transport may therefore be induced by a mechanism other than interaction with microtubules for the latter two agents; and potentially this alternate mechanism also contributes to suppression of axonal transport with other chemotherapeutics.
Loss of intraepidermal nerve fibers & Meissner’s corpuscle during CIPN
The cumulative effect of the above mechanisms appears to result in a loss of intraepidermal nerve fibers (IENFs) and Meissner’s corpuscles (MC) that appear in areas of skin where patients experience their most severe symptoms of CIPN. The observed loss of MCs explains the decreased touch perception of CIPN patients [1]. Palitaxel [98], oxaliplatin [99] and bortezomib [1] produce IENF loss at a time that corresponds to the peak of CIPN symptoms in humans and in animal models. Although the specific mechanisms driving this loss of IENF are unclear, similar findings are also seen in other diseases that result in painful neuropathy, such as HIV and diabetes [100,101]. Interestingly, prevention of IENF loss by the tetracycline derivative, minocycline, which reduces neuroinflammation, also protects against neuropathy produced by oxaliplatin [99] and paclitaxel [98] in animal models of CIPN. Similarly, interventions directed at the suppressing CCL2, a chemokine prominently involved in proinflammatory responses in dorsal root ganglia that are evoked by chemotherapy treatments, blocked both the behavioral signs of CIPN as well as reduced distal IENF density in rats [102].
Glial cell function
Much of the research on CIPN has focused on neuronal changes; however, the contributions of glial cells should not be overlooked. Changes to Schwann cells in the periphery, satellite cells in the DRG and astrocytes in the spinal cord seem to be an important component of CIPN. As noted above, inhibition of astrocyte glutamate transporters may be a common mechanism among chemotherapeutics in producing CIPN. But there are several other possible mechanisms where glial cells may play roles in the pathophysiology of CIPN. For example, following cisplatin or paclitaxel exposure, Schwann cells activate and begin to release inflammatory cytokines, such as TNF-α [103–105] (see more below). Following activation of apoptotic pathways, peripheral nerves experience a loss of Schwann cells [106], leading to a loss of protection and nourishment to nerve fibers and impairment of action potential propagation.
Likewise, satellite cells, when activated by chemotherapeutics, begin to secrete cytokines [107], which can contribute to apoptosis of DRG neurons. Satellite cells also experience an increase in gap junction coupling, and blocking this effect produced an analgesic response following chemotherapy-induced sensitization in mice [108].
Within the spinal cord, activation of astrocytes, but not microglia contributes to CIPN symptoms [109,110]. Astrocyte activation leads to increased cytokine release, which contributes to behaviors indicative of neuropathic pain in mice [111]. Decreasing astrocyte activation by treatment with minocycline or reducing gap junction coupling with carbenoxolone can decrease chemotherapy-induced mechanical hyperalgesia in rodents [38,112].
Cytokine & chemokine binding
Cytokines historically were viewed as small proteins released by cells of the immune system to promote immune responses such as fever and inflammation. It is now known that cytokines, including chemotactic cytokines (chemokines), are also released by glia and neurons, and these versatile signals have well-established roles in many forms of pain. Injection of proinflammatory cytokines produces a robust hypersensitivity to thermal and mechanical stimulation [113,114], and administration of cytokine receptor antagonists can mitigate hyperalgesia in the mouse [115]. Cytokines can enhance pain responding in a number ways in the peripheral nervous system. Direct sensitization of primary afferent fibers occurs following proinflammatory cytokine exposure, leading to spontaneous discharge [116]. This effect is also seen within the DRG [117] and in dorsal horn neurons [118] following cytokine exposure. TNF-α can decrease GABAergic inhibitory signaling in the spinal cord via a MAPK (p38)-mediated pathway to enhance pain signaling [119]. Cytokines can also indirectly lead to a host of inflammation-related responses, such as the release of bradykinin, serotonin and histamine [120]; and can activate apoptotic pathways within cells to contribute to pain [121].
Chemotherapeutic exposure consistently enhances cytokine release. Administration of paclitaxel [122], cisplatin [123] and vincristine [124] leads to the increased production and release of proinflammatory cytokines such as TNF-α and IL-1β and chemokines such as MCP-1. These cytokines can bind to receptors located on neurons and glial cells to enhance activity in pain pathways, and in turn, increase expression of cytokines in these same cells, thus leading to a potentially self-sustaining cycle [125].
One receptor important for regulating the release of cytokines shown to be involved in CIPN is the Toll-like receptor (TLR). Toll-like receptors are a family of pathogen-detecting transmembrane proteins that can be activated by chemotherapeutics [126]. While traditionally viewed as being primarily involved in innate immunity, the TLRs have also more recently been implicated in pain. Increased levels of TLR4 are expressed in the DRG of rats displaying paclitaxel-induced hyperalgesia, and that hyperalgesia is significantly ameliorated using an antagonist to TLR4 receptors (a lipopolysaccharide isolated from Rhodbacter sphaeroides) [127]. Complementary evidence for an important role of TLR signaling in CIPN came from observations of attenuated responses after cisplatin treatment in mice in which TLR4 or TLR3 were knocked out [128].
MCP1 (also called CCL2), a chemokine, and its receptor CCR2 have also been shown to be altered in CIPN. MCP1 is increased in spinal astrocytes and nociceptive DRG neurons in rats with paclitaxel-induced CIPN, and CCR2 numbers increased in large- and medium-sized DRG cells during paclitaxel-induced hyperalgesia [102]. Antagonism of CCR2 [129] mitigated neuropathic pain in mice, a finding similar to the effect of CCR2 gene knockout [130].
Conclusion
Chemotherapy remains a frontline treatment for many forms of cancer, but unfortunately is associated with the painful and debilitating condition of neuropathy. While research has provided insight into the mechanisms underlying this condition, treatment for CIPN is still limited. This is perhaps due in part to the complexity of these mechanisms. As outlined above, CIPN affects many aspects of neuronal and glial cell function, creating cascading effects and potentially engaging feedback loops that may sustain the neuropathy and pain.
Future perspective
Currently, clinical trials have not revealed effective treatments to prevent the development of CIPN, although many interventions have been tested, including ALCAR, vitamin E, infusions of calcium or magnesium ions, and amitriptyline [131]. Opiates, a mainstay for many forms of chronic pain, provides only limited relief for chemotherapy-induced pain, and does so at the risk of addiction. It is, therefore, important to find alternative treatments. Many of the mechanisms discussed here have been studied as potential avenues of CIPN treatment, but the clinical trials have produced mixed results. For example, inhibition of p38 MAPK was found to decrease pain associated with peripheral injury in one clinical trial [132] but not another [133]. When studying CIPN mechanisms and developing treatments on the basis of preclinical studies, it is important to keep in mind issues of validity and reliability, as was highlighted by the recent finding of species differences in the function of TRPA1 channels [58]. Future research should benefit from further consideration of the role of glial cells in CIPN. Finally, as a newer generation of chemotherapeutics becomes available, such as ixabepilone, researchers can compare and contrast prevalence of CIPN and associated mechanisms to help identify cellular and molecular contributions to CIPN.
Practice points.
Pharmacogenomics provides insights into potential genetic predictors for chemotherapy-induced peripheral neuropathy (CIPN).
Changes in cellular activation and signaling, including enhanced cytokine release, changes in voltage-gated ion channels, altered neurotransmission and activation of apoptotic pathways have been observed.
Structural changes to the cell, especially mitochondrial and microtubule damage, play a role in the chronicity of CIPN.
Loss of intraepidermal nerve fibers and Meissner’s corpuscles further contributes to the ongoing nature of this condition.
Glial cells are important contributors to CIPN. The most relevant of these cells are the astrocytes, satellite cells and Schwann cells.
Footnotes
Financial & competing interests disclosure
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
No writing assistance was utilized in the production of this manuscript.
References
Papers of special note have been highlighted as • of interest
- 1.Boyette-Davis JA, Cata JP, Zhang H, et al. Follow-up psychophysical studies in bortezomib-related chemoneuropathy patients. J. Pain. 2011;12(9):1017–1024. doi: 10.1016/j.jpain.2011.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bhatnagar B, Gilmore S, Goloubeva O, et al. Chemotherapy dose reduction due to chemotherapy induced peripheral neuropathy in breast cancer patients receiving chemotherapy in the neoadjuvant or adjuvant settings. a single-center experience. Springerplus. 2014;3:366. doi: 10.1186/2193-1801-3-366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cavaletti G, Bogliun G, Marzorati L, et al. Peripheral neurotoxicity of taxol in patients previously treated with cisplatin. Cancer. 1995;75:1141–1150. doi: 10.1002/1097-0142(19950301)75:5<1141::aid-cncr2820750514>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- 4.Kroigard T, Schroder HD, Qvortrup C, et al. Characterization and diagnostic evaluation of chronic polyneuropathies induced by oxaliplatin and docetaxel comparing skin biopsy to quantitative sensory testing and nerve conduction studies. Eur. J. Neurol. 2014;21(4):623–629. doi: 10.1111/ene.12353. [DOI] [PubMed] [Google Scholar]
- 5.de Carvalho Barbosa M, Kosturakis AK, Eng C, et al. Quantitative sensory analysis of peripheral neuropathy produced by colorectal cancer and its exacerbation by cumulative dose of oxaliplatin chemotherapy. Cancer Res. 2014;74(21):5955–5962. doi: 10.1158/0008-5472.CAN-14-2060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Postma TJ, Benard BA, Huijgens PC, Ossenkoppele GJ, Heimans JJ. Long term effects of vincristine on the peripheral nervous system. J. Neuroonocol. 1993;15:23–27. doi: 10.1007/BF01050259. [DOI] [PubMed] [Google Scholar]
- 7.Dougherty PM, Cata JP, Burton AW, Vu K, Weng HR. Dysfunction in multiple primary afferent fiber subtypes revealed by quantitative sensory testing in patients with chronic vincristine-induced pain. J. Pain Symptom Manage. 2007;33(2):166–179. doi: 10.1016/j.jpainsymman.2006.08.006. [DOI] [PubMed] [Google Scholar]
- 8.Dougherty PM, Cata JP, Cordella JV, Burton A, Weng H-R. Taxol-induced sensory disturbance is characterized by preferential impairment of myelinated fiber function in cancer patients. Pain. 2004;109:132–142. doi: 10.1016/j.pain.2004.01.021. [DOI] [PubMed] [Google Scholar]
- 9.Grisold W, Cavaletti G, Windebank AJ. Peripheral neuropathies from chemotherapeutics and targeted agents: diagnosis, treatment, and prevention. Neuro Oncol. 2012;14(Suppl. 4):iv45–iv54. doi: 10.1093/neuonc/nos203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Boyette-Davis JA, Cata JP, Driver LC, et al. Persistent chemoneuropathy in patients receiving the plant alkaloids paclitaxel and vincristine. Cancer Chemother. Pharmacol. 2013;71:619–626. doi: 10.1007/s00280-012-2047-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mols F, Beijers T, Vreugdenhil G, Poll-Franse L. Chemotherapy-induced peripheral neuropathy and its association with quality of life: a systematic review. Support. Care Cancer. 2014;22(8):2261–2269. doi: 10.1007/s00520-014-2255-7. [DOI] [PubMed] [Google Scholar]
- 12.Cavaletti G, Alberti P, Marmiroli P. Chemotherapy-induced peripheral neurotoxicity in the era of pharmacogenomics. Lancet Oncol. 2011;12(12):1151–1161. doi: 10.1016/S1470-2045(11)70131-0. [DOI] [PubMed] [Google Scholar]
- 13.Stoehlmacher J, Park DJ, Zhang W, et al. Association between glutathione S-transferase P1, T1, and M1 genetic polymorphism and survival of patients with metastatic colorectal cancer. J. Natl Cancer Inst. 2002;94(12):936–942. doi: 10.1093/jnci/94.12.936. [DOI] [PubMed] [Google Scholar]
- 14.Chen YC, Tzeng CH, Chen PM, et al. Influence of GSTP1 I105V polymorphism on cumulative neuropathy and outcome of FOLFOX-4 treatment in Asian patients with colorectal carcinoma. Cancer Sci. 2010;101(2):530–535. doi: 10.1111/j.1349-7006.2009.01418.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kanai M, Yoshioka A, Tanaka S, et al. Associations between glutathione S-transferase pi Ile105Val and glyoxylate aminotransferase Pro11Leu and Ile340Met polymorphisms and early-onset oxaliplatin-induced neuropathy. Cancer Epidemiol. 2010;34(2):189–193. doi: 10.1016/j.canep.2010.02.008. [DOI] [PubMed] [Google Scholar]
- 16.Won HH, Lee J, Park JO, et al. Polymorphic markers associated with severe oxaliplatin-induced, chronic peripheral neuropathy in colon cancer patients. Cancer. 2012;118(11):2828–2836. doi: 10.1002/cncr.26614. [DOI] [PubMed] [Google Scholar]; • Reported on single nucleotide polymorphisms that have significant predictive validity for chemotherapy-induced peripheral neuropathy (CIPN) development.
- 17.Beutler AS, Kulkarni AA, Kanwar R, et al. Sequencing of Charcot-Marie-Tooth disease genes in a toxic polyneuropathy. Ann. Neurol. 2014;76(5):727–737. doi: 10.1002/ana.24265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Grolleau F, Gamelin L, Boisdron-Celle M, Lapied B, Pelhate M, Gamelin E. A possible explanation for a neurotoxic effect of the anticancer agent oxaliplatin on neuronal voltage-gated sodium channels. J. Neurophysiol. 2001;85(5):2293–2297. doi: 10.1152/jn.2001.85.5.2293. [DOI] [PubMed] [Google Scholar]
- 19.Webster RG, Brain KL, Wilson RH, Grem JL, Vincent A. Oxaliplatin induces hyperexcitability at motor and autonomic neuromuscular junctions through effects on voltage-gated sodium channels. Br. J. Pharmacol. 2005;146(7):1027–1039. doi: 10.1038/sj.bjp.0706407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Park SB, Goldstein D, Lin CS, Krishnan AV, Friedlander ML, Kiernan MC. Acute abnormalities of sensory nerve function associated with oxaliplatin-induced neurotoxicity. J. Clin. Oncol. 2009;27(8):1243–1249. doi: 10.1200/JCO.2008.19.3425. [DOI] [PubMed] [Google Scholar]
- 21.Park SB, Lin CS, Krishnan AV, Goldstein D, Friedlander ML, Kiernan MC. Oxaliplatin-induced neurotoxicity: changes in axonal excitability precede development of neuropathy. Brain. 2009;132(Pt 10):2712–2723. doi: 10.1093/brain/awp219. [DOI] [PubMed] [Google Scholar]
- 22.Grothey A. Clinical management of oxaliplatin-associated neurotoxicity. Clin. Colorectal Cancer. 2005;(5 Suppl. 1):S38–S46. doi: 10.3816/ccc.2005.s.006. [DOI] [PubMed] [Google Scholar]
- 23.Lehky TJ, Leonard GD, Wilson RH, Grem JL, Floeter MK. Oxaliplatin-induced neurotoxicity: acute hyperexcitability and chronic neuropathy. Muscle Nerve. 2004;29(3):387–392. doi: 10.1002/mus.10559. [DOI] [PubMed] [Google Scholar]
- 24.Thibault K, Calvino B, Dubacq S, et al. Cortical effect of oxaliplatin associated with sustained neuropathic pain: exacerbation of cortical activity and down-regulation of potassium channel expression in somatosensory cortex. Pain. 2012;153(8):1636–1647. doi: 10.1016/j.pain.2012.04.016. [DOI] [PubMed] [Google Scholar]
- 25.Descoeur J, Pereira V, Pizzoccaro A, et al. Oxaliplatin-induced cold hypersensitivity is due to remodelling of ion channel expression in nociceptors. EMBO Mol. Med. 2011;3(5):266–278. doi: 10.1002/emmm.201100134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhang H, Dougherty PM. Enhanced excitability of primary sensory neurons and altered gene expression of neuronal ion channels in dorsal root ganglion in paclitaxel-induced peripheral neuropathy. Anesthesiology. 2014;120(6):1463–1475. doi: 10.1097/ALN.0000000000000176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Emery EC, Young GT, Berrocoso EM, Chen L, McNaughton PA. HCN2 ion channels play a central role in inflammatory and neuropathic pain. Science. 2011;333(6048):1462–1466. doi: 10.1126/science.1206243. [DOI] [PubMed] [Google Scholar]
- 28.Dimitrov AG, Dimitrova NA. A possible link of oxaliplatin-induced neuropathy with potassium channel deficit. Muscle Nerve. 2012;45(3):403–411. doi: 10.1002/mus.22311. [DOI] [PubMed] [Google Scholar]
- 29.Nodera H, Spieker A, Sung M, Rutkove S. Neuroprotective effects of Kv7 channel agonist, retigabine, for cisplatin-induced peripheral neuropathy. Neurosci. Lett. 2011;505(3):223–227. doi: 10.1016/j.neulet.2011.09.013. [DOI] [PubMed] [Google Scholar]
- 30.Matsumoto M, Inoue M, Hald A, Xie W, Ueda H. Inhibition of paclitaxel-induced A-fiber hypersensitization by gabapentin. J. Pharmacol. Exp. Ther. 2006;318(2):735–740. doi: 10.1124/jpet.106.103614. [DOI] [PubMed] [Google Scholar]
- 31.Flatters SJL, Bennett GJ. Ethosuximide reverses paclitaxel- and vincristine-induced painful peripheral neuropathy. Pain. 2004;109(1–2):150–161. doi: 10.1016/j.pain.2004.01.029. [DOI] [PubMed] [Google Scholar]
- 32.Xiao W, Boroujerdi A, Bennett GJ, Luo ZD. Chemotherapy-evoked painful peripheral neuropathy: analgesic effects of gabapentin and effects on expression of the alpha-2-delta type-1 calcium channel subunit. Neuroscience. 2007;144(2):714–720. doi: 10.1016/j.neuroscience.2006.09.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Thibault K, Van Steenwinckel J, Brisorgueil MJ, et al. Serotonin 5-HT2A receptor involvement and Fos expression at the spinal level in vincristine-induced neuropathy in the rat. Pain. 2008;140(2):305–322. doi: 10.1016/j.pain.2008.09.006. [DOI] [PubMed] [Google Scholar]
- 34.Hansen N, Uceyler N, Palm F, et al. Serotonin transporter deficiency protects mice from mechanical allodynia and heat hyperalgesia in vincristine neuropathy. Neurosci. Lett. 2011;495(2):93–97. doi: 10.1016/j.neulet.2011.03.035. [DOI] [PubMed] [Google Scholar]
- 35.Carozzi VA, Canta A, Chiorazzi A, Cavaletti G. Chemotherapy-induced peripheral neuropathy: What do we know about mechanisms? Neurosci. Lett. 2014 doi: 10.1016/j.neulet.2014.10.014. [DOI] [PubMed] [Google Scholar]
- 36.Ghelardini C, Menicacci C, Cerretani D, Bianchi E. Spinal administration of mGluR5 antagonist prevents the onset of bortezomib induced neuropathic pain in rat. Neuropharmacology. 2014;86:294–300. doi: 10.1016/j.neuropharm.2014.08.004. [DOI] [PubMed] [Google Scholar]
- 37.Matute C, Domercq M, Sanchez-Gomez MV. Glutamate-mediated glial injury: mechanisms and clinical importance. GLIA. 2006;53(2):212–224. doi: 10.1002/glia.20275. [DOI] [PubMed] [Google Scholar]
- 38.Robinson CR, Dougherty PM. Spinal astrocute gap junction and glutamate transporter expression contributes to a rat model of bortezomib-induced peripheral neuropathy. Neuroscience. 2015;285(1):1–10. doi: 10.1016/j.neuroscience.2014.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cata JP, Weng HR, Chen JH, Dougherty PM. Altered discharges of spinal wide dynamic range neurons and down-regulation of glutamate transporter expression in rats with paclitaxel-induced hyperalgesia. Neuroscience. 2006;138(1):329–338. doi: 10.1016/j.neuroscience.2005.11.009. [DOI] [PubMed] [Google Scholar]
- 40.Cata JP, Weng H-R, Dougherty PM. Behavioral and electrophysiological studies in rats with cisplatin-induced chemoneuropathy. Brain Res. 2008;1230:91–98. doi: 10.1016/j.brainres.2008.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Weng H-R, Cordella JV, Dougherty PM. Changes in sensory processing in the spinal dorsal horn accompany vincristine-induced hyperalgesia and allodynia. Pain. 2003;103:131–138. doi: 10.1016/s0304-3959(02)00445-1. [DOI] [PubMed] [Google Scholar]
- 42.Yang Y, Zhang YG, Lin GA, et al. Spinal changes of a newly isolated neuropeptide endomorphin-2 concomitant with vincristine-induced allodynia. PLoS ONE. 2014;9(2):e89583. doi: 10.1371/journal.pone.0089583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Guindon J, Lai Y, Takacs SM, Bradshaw HB, Hohmann AG. Alterations in endocannabinoid tone following chemotherapy-induced peripheral neuropathy: effects of endocannabinoid deactivation inhibitors targeting fatty-acid amide hydrolase and monoacylglycerol lipase in comparison to reference analgesics following cisplatin treatment. Pharmacol. Res. 2013;67(1):94–109. doi: 10.1016/j.phrs.2012.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Uhelski ML, Khasabova IA, Simone DA. Inhibition of anandamide hydrolysis attenuates nociceptor sensitization in a murine model of chemotherapy-induced peripheral neuropathy. J. Neurophysiol. 2015;113(5):1501–1510. doi: 10.1152/jn.00692.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Janes K, Esposito E, Doyle T, et al. A3 adenosine receptor agonist prevents the development of paclitaxel-induced neuropathic pain by modulating spinal glial-restricted redox-dependent signaling pathways. Pain. 2015;155:2560–2567. doi: 10.1016/j.pain.2014.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Nagy I, Friston D, Valente JS, Torres Perez JV, Andreou AP. Pharmacology of the capsaicin receptor, transient receptor potential vanilloid type-1 ion channel. Prog. Drug Res. 2014;68:39–76. doi: 10.1007/978-3-0348-0828-6_2. [DOI] [PubMed] [Google Scholar]
- 47.Simone DA, Baumann TK, LaMotte RH. Dose-dependent pain and mechanical hyperalgesia in humans after intradermal injection of capsaicin. Pain. 1989;38:99–107. doi: 10.1016/0304-3959(89)90079-1. [DOI] [PubMed] [Google Scholar]
- 48.Marchettini P, Simone DA, Caputi G, Ochoa JL. Pain from excitation of identified muscle nociceptors in humans. Brain Res. 1996;740(1–2):109–116. doi: 10.1016/s0006-8993(96)00851-7. [DOI] [PubMed] [Google Scholar]
- 49.Witting N, Svensson P, Gottrup H, Arendt-Nielsen L, Jensen TS. Intramuscular and intradermal injection of capsaicin: a comparison of local and referred pain. Pain. 2000;84(2–3):407–412. doi: 10.1016/s0304-3959(99)00231-6. [DOI] [PubMed] [Google Scholar]
- 50.Hara T, Chiba T, Abe K, et al. Effect of paclitaxel on transient receptor potential vallinoid 1 in rat dorsal root ganglion. Pain. 2013;154:882–889. doi: 10.1016/j.pain.2013.02.023. [DOI] [PubMed] [Google Scholar]
- 51.Quartu M, Carozzi VA, Dorsey SG, et al. Bortezomib treatment produces nocifensive behavior and changes in the expression of TRPV1, CGRP, and substance P in the rat DRG, spinal cord, and sciatic nerve. Biomed. Res. Int. 2014;2014:180428. doi: 10.1155/2014/180428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ta LE, Bieber AJ, Carlton SM, Loprinzi CL, Low PA, Windebank AJ. Transient Receptor Potential Vanilloid 1 is essential for cisplatin-induced heat hyperalgesia in mice. Mol. Pain. 2010;6:15. doi: 10.1186/1744-8069-6-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Laursen WJ, Bagriantsev SN, Gracheva EO. TRPA1 channels: chemical and temperature sensitivity. Curr. Top. Membr. 2014;74:89–112. doi: 10.1016/B978-0-12-800181-3.00004-X. [DOI] [PubMed] [Google Scholar]
- 54.Wei H, Koivisto A, Saarnilehto M, et al. Spinal transient receptor potential ankyrin 1 channel contributes to central pain hypersensitivity in various pathophysiological conditions in the rat. Pain. 2011;152(3):582–591. doi: 10.1016/j.pain.2010.11.031. [DOI] [PubMed] [Google Scholar]
- 55.Nassini R, Gees M, Harrison S, et al. Oxaliplatin elicits mechanical and cold allodynia in rodents via TRPA1 receptor stimulation. Pain. 2011;152(7):1621–1631. doi: 10.1016/j.pain.2011.02.051. [DOI] [PubMed] [Google Scholar]
- 56.Zhao M, Isami K, Nakamura S, Shirakawa H, Nakagawa T, Kaneko S. Acute cold hypersensitivity characteristically induced by oxaliplatin is caused by the enhanced responsiveness of TRPA1 in mice. Mol. Pain. 2012;8:55. doi: 10.1186/1744-8069-8-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Materazzi S, Fusi C, Benemei S, et al. TRPA1 and TRPV4 mediate paclitaxel-induced peripheral neuropathy in mice via a glutathione-sensitive mechanism. Pflugers Arch. 2012;463:561–569. doi: 10.1007/s00424-011-1071-x. [DOI] [PubMed] [Google Scholar]
- 58.Chen J, Kang D, Xu J, et al. Species differences and molecular determinant of TRPA1 cold sensitivity. Nat. Commun. 2013;4:2501. doi: 10.1038/ncomms3501. [DOI] [PMC free article] [PubMed] [Google Scholar]; • Species differences and molecular determinant of TRPA1 cold sensitivity.
- 59.Chen Y, Yang C, Wang ZJ. Proteinase-activated receptor 2 sensitizes transient receptor potential vanilloid 1, transient receptor potential vanilloid 4, and transient receptor potential ankyrin 1 in paclitaxel-induced neuropathic pain. Neuroscience. 2011;193:440–451. doi: 10.1016/j.neuroscience.2011.06.085. [DOI] [PubMed] [Google Scholar]
- 60.Peier AM, Reeve AJ, Andersson DA, et al. A heat-sensitive TRP channel expressed in keratinocytes. Science. 2002;296:2046–2049. doi: 10.1126/science.1073140. [DOI] [PubMed] [Google Scholar]
- 61.Proudfoot CJ, Garry EM, Cottrell DF, et al. Analgesia mediated by the TRPM8 cold receptor in chronic neuropathic pain. Curr. Biol. 2006;16(16):1591–1605. doi: 10.1016/j.cub.2006.07.061. [DOI] [PubMed] [Google Scholar]
- 62.Storey DJ, Colvin LA, Mackean MJ, Mitchell R, Fleetwood-Walker SM, Fallon MT. Reversal of dose-limiting carboplatin-induced peripheral neuropathy with TRM8 activator menthol, enables further effective chemotherapy delivery. J. Pain Symptom. Manag. 2010;39(6):e2–e4. doi: 10.1016/j.jpainsymman.2010.02.004. [DOI] [PubMed] [Google Scholar]
- 63.Park SJ, Wu CH, Gordon JD, Zhong X, Emami A, Safa AR. Taxol induces caspase-10-dependent apoptosis. J. Biol. Chem. 2004;279(49):51057–51067. doi: 10.1074/jbc.M406543200. [DOI] [PubMed] [Google Scholar]
- 64.Joseph EK, Levine JD. Comparison of oxaliplatin- and cisplatin-induced painful peripheral neuropathy in the rat. J. Pain. 2009;10(5):534–541. doi: 10.1016/j.jpain.2008.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Joseph EK, Levine JD. Caspase signalling in neuropathic and inflammatory pain in the rat. Eur. J. Neurosci. 2004;20(11):2896–2902. doi: 10.1111/j.1460-9568.2004.03750.x. [DOI] [PubMed] [Google Scholar]
- 66.Ta LE, Espeset L, Podratz J, Windebank AJ. Neurotoxicity of oxaliplatin and cisplatin for dorsal root ganglion neurons correlates with platinum-DNA binding. Neurotoxicology. 2006;27(6):992–1002. doi: 10.1016/j.neuro.2006.04.010. [DOI] [PubMed] [Google Scholar]
- 67.Scuteri A, Galimberti A, Maggioni D, et al. Role of MAPKs in platinum-induced neuronal apoptosis. Neurotoxicology. 2009;30(2):312–319. doi: 10.1016/j.neuro.2009.01.003. [DOI] [PubMed] [Google Scholar]
- 68.Scuteri A, Galimberti A, Ravasi M, et al. NGF protects dorsal root ganglion neurons from oxaliplatin by modulating JNK/Sapk and ERK1/2. Neurosci. Lett. 2010;486(3):141–145. doi: 10.1016/j.neulet.2010.09.028. [DOI] [PubMed] [Google Scholar]
- 69.Flatters SJ, Bennett GJ. Studies of peripheral sensory nerves in paclitaxel-induced painful peripheral neuropathy: evidence for mitochondrial dysfunction. Pain. 2006;122(3):245–257. doi: 10.1016/j.pain.2006.01.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Xiao WH, Zheng H, Zheng FY, Nuydens R, Meert TF, Bennett GJ. Mitochondrial abnormality in sensory, but not motor, axons in paclitaxel-evoked painful peripheral neuropathy in the rat. Neuroscience. 2011;199:461–469. doi: 10.1016/j.neuroscience.2011.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Zheng H, Xiao WH, Bennett GJ. Functional deficits in peripheral nerve mitochondria in rats with paclitaxel- and oxaliplatin-evoked painful peripheral neuropathy. Exp. Neurol. 2011;232(2):154–161. doi: 10.1016/j.expneurol.2011.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Xiao WH, Bennett GJ. Effects of mitochondrial poisons on the neuropathic pain produced by the chemotherapeutic agents paclitaxel and oxaliplatin. Pain. 2012;153:704–709. doi: 10.1016/j.pain.2011.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Zheng H, Xiao WH, Bennett GJ. Mitotoxicity and bortezomib-induced chronic painful peripheral neuropathy. Exp. Neurol. 2012;238(2):225–234. doi: 10.1016/j.expneurol.2012.08.023. [DOI] [PubMed] [Google Scholar]
- 74.Flatters SJ, Xiao WH, Bennett GJ. Acetyl-L-carnitine prevents and reduces paclitaxel-induced painful peripheral neuropathy. Neurosci. Lett. 2006;397(3):219–223. doi: 10.1016/j.neulet.2005.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]; • Indicated ALCAR as a potential prevention of CIPN.
- 75.Pisano C, Pratesi G, Laccabue D, et al. Paclitaxel and cisplatin-induced neurotoxicity: a protective role of acetyl-L-carnitine. Clin. Cancer Res. 2003;9(15):5756–5767. [PubMed] [Google Scholar]
- 76.Ghirardi O, Lo GP, Pisano C, et al. Acetyl-L-Carnitine prevents and reverts experimental chronic neurotoxicity induced by oxaliplatin, without altering its antitumor properties. Anticancer Res. 2005;25(4):2681–2687. [PubMed] [Google Scholar]
- 77.Jin HW, Flatters SJ, Xiao WH, Mulhern HL, Bennett GJ. Prevention of paclitaxel-evoked painful peripheral neuropathy by acetyl-L-carnitine: effects on axonal mitochondria, sensory nerve fiber terminal arbors, and cutaneous Langerhans cells. Exp. Neurol. 2008;210(1):229–237. doi: 10.1016/j.expneurol.2007.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Bianchi G, Vitali G, Caraceni A, et al. Symptomatic and neurophysiological responses of paclitaxel- or cisplatin-induced neuropathy to oral acetyl-L-carnitine. Eur. J. Cancer. 2005;41(12):1746–1750. doi: 10.1016/j.ejca.2005.04.028. [DOI] [PubMed] [Google Scholar]
- 79.Maestri A, De Pasquale CA, Cundari S, Zanna C, Cortesi E, Crino L. A pilot study on the effect of acetyl-L-carnitine in paclitaxel- and cisplatin-induced peripheral neuropathy. Tumori. 2005;91(2):135–138. doi: 10.1177/030089160509100206. [DOI] [PubMed] [Google Scholar]
- 80.Callander N, Markovina S, Eickhoff J, et al. Acetyl-L-carnitine (ALCAR) for the prevention of chemotherapy-induced peripheral neuropathy in patients with relapsed or refractory multiple myeloma treated with bortezomib, doxorubicin and low-dose dexamethasone: a study from the Wisconsin Oncology Network. Cancer Chemother. Pharmacol. 2014;74(4):875–882. doi: 10.1007/s00280-014-2550-5. [DOI] [PMC free article] [PubMed] [Google Scholar]; • Clinical trial that did not find significant prevention of CIPN with ALCAR.
- 81.Hershman DL, Unger JM, Crew KD, et al. Randomized double-blind placebo-controlled trial of acetyl-L-carnitine for the prevention of taxane-induced neuropathy in women undergoing adjuvant breast cancer therapy. J. Clin. Oncol. 2013;31(20):2627–2633. doi: 10.1200/JCO.2012.44.8738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Hui KF, Lam BH, Ho DN, Tsao SW, Chiang AK. Bortezomib and SAHA synergistically induce ROS-driven caspase-dependent apoptosis of nasopharyngeal carcinoma and block replication of Epstein-Barr virus. Mol. Cancer Ther. 2013;12(5):747–758. doi: 10.1158/1535-7163.MCT-12-0811. [DOI] [PubMed] [Google Scholar]
- 83.Barriere DA, Rieusset J, Chanteranne D, et al. Paclitaxel therapy potentiates cold hyperalgesia in streptozotocin-induced diabetic rats through enhanced mitochondrial reactive oxygen species production and TRPA1 sensitization. Pain. 2012;153(3):553–561. doi: 10.1016/j.pain.2011.11.019. [DOI] [PubMed] [Google Scholar]
- 84.Kim HK, Zhang YP, Gwak YS, Abdi S. Phenyl N-tert-butylnitrone, a free radical scavenger, reduces mechanical allodynia in chemotherapy-induced neuropathic pain in rats. Anesthesiology. 2010;112(2):432–439. doi: 10.1097/ALN.0b013e3181ca31bd. [DOI] [PubMed] [Google Scholar]
- 85.Fidanboylu M, Griffiths LA, Flatters SJ. Global inhibition of reactive oxygen species (ROS) inhibits paclitaxel-induced painful peripheral neuropathy. PLoS ONE. 2011;6(9):e25212. doi: 10.1371/journal.pone.0025212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Doyle T, Chen Z, Muscoli C, et al. Targeting the overproduction of peroxynitrite for the prevention and reversal of paclitaxel-induced neuropathic pain. J. Neurosci. 2012;32(18):6149–6160. doi: 10.1523/JNEUROSCI.6343-11.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Areti A, Yerra VG, Naidu V, Kumar A. Oxidative stress and nerve damage: role in chemotherapy induced peripheral neuropathy. Redox. Biol. 2014;2:289–295. doi: 10.1016/j.redox.2014.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Kelley MR, Jiang Y, Guo C, Reed A, Meng H, Vasko MR. Role of the DNA base excision repair protein, APE1 in cisplatin, oxaliplatin, or carboplatin induced sensory neuropathy. PLoS ONE. 2014;9(9):e106485. doi: 10.1371/journal.pone.0106485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Santin G, Scietti L, Veneroni P, Barni S, Bernocchi G, Bottone MG. Effects of Cisplatin in neuroblastoma rat cells: damage to cellular organelles. Int. J. Cell Biol. 2012;2012:424072. doi: 10.1155/2012/424072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Santin G, Piccolini VM, Veneroni P, Barni S, Bernocchi G, Bottone MG. Different patterns of apoptosis in response to cisplatin in B50 neuroblastoma rat cells. Histol. Histopathol. 2011;26(7):831–842. doi: 10.14670/HH-26.831. [DOI] [PubMed] [Google Scholar]
- 91.Shin YK, Jang SY, Lee HK, et al. Pathological adaptive responses of Schwann cells to endoplasmic reticulum stress in bortezomib-induced peripheral neuropathy. GLIA. 2010;58(16):1961–1976. doi: 10.1002/glia.21065. [DOI] [PubMed] [Google Scholar]
- 92.Argyriou AA, Polychronopoulos P, Iconomou G, et al. Incidence and characteristics of peripheral neuropathy during oxaliplatin-based chemotherapy for metastatic colon cancer. Acta Oncol. 2007;46(8):1131–1137. doi: 10.1080/02841860701355055. [DOI] [PubMed] [Google Scholar]
- 93.Carlson K, Ocean AJ. Peripheral neuropathy with microtubule-targeting agents: occurrence and management approach. Clin. Breast Cancer. 2011;11(2):73–81. doi: 10.1016/j.clbc.2011.03.006. [DOI] [PubMed] [Google Scholar]
- 94.Lee JJ, Swain SM. Peripheral neuropathy induced by microtubule-stabilizing agents. J. Clin. Oncol. 2006;24(10):1633–1642. doi: 10.1200/JCO.2005.04.0543. [DOI] [PubMed] [Google Scholar]
- 95.LaPointe NE, Morfini G, Brady ST, Feinstein SC, Wilson L, Jordan MA. Effects of eribulin, vincristine, paclitaxel and ixabepilone on fast axonal transport and kinesin-1 driven microtubule gliding: implications for chemotherapy-induced peripheral neuropathy. Neurotoxicology. 2013;37:231–239. doi: 10.1016/j.neuro.2013.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Staff NP, Podratz JL, Grassner L, et al. Bortezomib alters microtubule polymerization and axonal transport in rat dorsal root ganglion neurons. Neurotoxicology. 2013;39:124–131. doi: 10.1016/j.neuro.2013.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Schellingerhout D, LeRoux LG, Hobbs BP, Bredow S. Impairment of retrograde neuronal transport in oxaliplatin-induced neuropathy demonstrated by molecular imaging. PLoS ONE. 2012;7(9):e45776. doi: 10.1371/journal.pone.0045776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Boyette-Davis J, Xin W, Zhang H, Dougherty PM. Intraepidermal nerve fiber loss corresponds to the development of Taxol-induced hyperalgesia and can be prevented by treatment with minocycline. Pain. 2011;152(2):308–313. doi: 10.1016/j.pain.2010.10.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Boyette-Davis J, Dougherty PM. Protection against oxaliplatin-induced mechanical hyperalgesia and intraepidermal nerve fiber loss by minocycline. Exp. Neurol. 2011;229(2):353–357. doi: 10.1016/j.expneurol.2011.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Lehmann HC, Chen W, Borzan J, Mankowski JL, Hoke A. Mitochondrial dysfunction in distal axons contributes to human immunodeficiency virus sensory neuropathy. Ann. Neurol. 2011;69(1):100–110. doi: 10.1002/ana.22150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Oaklander AL. The density of remaining nerve endings in human skin with and without postherpetic neuralgia after shingles. Pain. 2001;92(1–2):139–145. doi: 10.1016/s0304-3959(00)00481-4. [DOI] [PubMed] [Google Scholar]
- 102.Zhang H, Boyette-Davis JA, Kosturakis AK, et al. Induction of monocyte chemoattractant protein-1 (MCP-1) and its receptor CCR2 in primary sensory neurons contributes to paclitaxel-induced peripheral neuropathy. J. Pain. 2013;14(10):1031–1044. doi: 10.1016/j.jpain.2013.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Cata JP, Weng H-R, Dougherty PM. Clinical and experimental findings in humans and animals with chemotherapy-induced peripheral neuropathy. Minerva Anes. 2006;72:151–169. [PubMed] [Google Scholar]
- 104.Cavaletti G, Cavaletti E, Oggioni N, et al. Distribution of paclitaxel within the nervous system of the rat after repeated intravenous administration. Neurotoxicology. 2000;21(3):389–394. [PubMed] [Google Scholar]
- 105.Ozturk G, Erdogan E, Anlar O, Kosem M, TaspInar M. Effect of leukemia inhibitory factor in experimental cisplatin neuropathy in mice. Cytokine. 2005;29(1):31–41. doi: 10.1016/j.cyto.2004.09.006. [DOI] [PubMed] [Google Scholar]
- 106.Cliffer KD, Siuciak JA, Carson SR, et al. Physiological characterization of taxol-induced large fiber sensory neuropathy in the rat. Ann. Neurol. 1998;43:46–55. doi: 10.1002/ana.410430111. [DOI] [PubMed] [Google Scholar]
- 107.Takeda M, Tanimoto T, Kadoi J, et al. Enhanced excitability of nociceptive trigeminal ganglion neurons by satellite glial cytokine following peripheral inflammation. Pain. 2007;129(1–2):155–166. doi: 10.1016/j.pain.2006.10.007. [DOI] [PubMed] [Google Scholar]
- 108.Warwick RA, Hanani M. The contribution of satellite glial cells to chemotherapy-induced neuropathic pain. Eur. J. Pain. 2013;17:571–580. doi: 10.1002/j.1532-2149.2012.00219.x. [DOI] [PubMed] [Google Scholar]
- 109.Zhang H, Yoon S-Y, Zhang H, Dougherty PM. Evidence that spinal astrocytes but not microglia contribute to the pathogenesis of paclitaxel-induced painful neuropathy. J. Pain. 2012;13(3):293–303. doi: 10.1016/j.jpain.2011.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Robinson CR, Zhang H, Dougherty PM. Astrocytes, but not microglia, are activated in oxaliplatin and bortezomib-induced peripheral neuropathy. Neuroscience. 2014;274(1):308–317. doi: 10.1016/j.neuroscience.2014.05.051. [DOI] [PMC free article] [PubMed] [Google Scholar]; • Bortezomib results in mechanical hyperalgesia via decreased glutamate transporter expression and increased astrocytic gap junction coupling.
- 111.Gao YJ, Zhang L, Samad OA, et al. JNK-Induced MCP-1 Production in spinal cord astrocytes contributes to central sensitization and neuropathic pain. J. Neurosci. 2009;29(13):4096–4108. doi: 10.1523/JNEUROSCI.3623-08.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Yoon S-Y, Robinson CR, Zhang H, Dougherty PM. Gap junction protein connexin 43 is involved in the induction of oxaliplatin-related neuropathic pain. J. Pain. 2013;14(2):205–214. doi: 10.1016/j.jpain.2012.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Woolf CJ, Allchorne A, Safieh-Garabedian B, Poole S. Cytokines, nerve growth factor and inflammatory hyperalgesia: the contribution of tumor necrosis factor a. Br. J. Pharmacol. 1997;121:417–424. doi: 10.1038/sj.bjp.0701148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Binshtok AM, Wang H, Zimmermann K, et al. Nociceptors Are Interleukin-1 beta Sensors. J. Neurosci. 2008;28(52):14062–14073. doi: 10.1523/JNEUROSCI.3795-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Cunha JM, Cunha FQ, Poole S, Ferreira SH. Cytokine-mediated inflammatory hyperalgesia limited by interleukin-1 receptor antagonist. Br. J. Pharmacol. 2000;130(6):1418–1424. doi: 10.1038/sj.bjp.0703434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Sorkin LS, Xaio W-H, Wagner R, Myers RR. Tumour necrosis factor-a induces ectopic activity in nociceptive primary afferent fibres. Neuroscience. 1997;81(1):255–262. doi: 10.1016/s0306-4522(97)00147-4. [DOI] [PubMed] [Google Scholar]
- 117.Ozaktay AC, Cavanaugh JM, Asik I, DeLeo JA, Weinstein JN. Dorsal root sensitivity to interleukin-1 beta, interleukin-6 and tumor necrosis factor in rats. Eur. Spine J. 2002;11:467–475. doi: 10.1007/s00586-002-0430-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Onda A, Hamba M, Yabuki S, Kikuchi S. Exogenous tumor necrosis factor-alpha induces abnormal discharges in rat dorsal horn neurons. Spine (Phila Pa 1976.) 2002;27(15):1618–1624. doi: 10.1097/00007632-200208010-00005. [DOI] [PubMed] [Google Scholar]
- 119.Zhang H, Nei H, Dougherty PM. A p38 mitogen-activated protein kinase-dependent mechanism of disinhibition in spinal synaptic transmission induced by tumor necrosis factor-alpha. J. Neurosci. 2010;30(38):12844–12855. doi: 10.1523/JNEUROSCI.2437-10.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.McMahon SB, Cafferty WB, Marchand F. Immune and glial cell factors as pain mediators and modulators. Exp. Neurol. 2005;192(2):444–462. doi: 10.1016/j.expneurol.2004.11.001. [DOI] [PubMed] [Google Scholar]
- 121.Vetere A, Choudhary A, Burns SM, Wagner BK. Targeting the pancreatic b-cell to treat diabetes. Nat. Rev. Drug Discov. 2014;13(4):278–289. doi: 10.1038/nrd4231. [DOI] [PubMed] [Google Scholar]
- 122.Zaks-Zilberman M, Zaks TZ, Vogel SN. Induction of proinflammatory and chemokine genes by lipopolysaccharide and paclitaxel (Taxol) in murine and human breast cancer cell lines. Cytokine. 2001;15(3):156–165. doi: 10.1006/cyto.2001.0935. [DOI] [PubMed] [Google Scholar]
- 123.Basu S, Sodhi A. Increased release of interleukin-1 and tumour necrosis factor by interleukin-2-induced lymphokine-activated killer cells in the presence of cisplatin and FK-565. Immunol. Cell Biol. 1992;70(Pt 1):15–24. doi: 10.1038/icb.1992.3. [DOI] [PubMed] [Google Scholar]
- 124.Weintraub M, Adde MA, Venzon DJ, et al. Severe atypical neuropathy associated with administration of hematopoietic colony-stimulating factors and vincristine. J. Clin. Oncol. 1996;14(3):935–940. doi: 10.1200/JCO.1996.14.3.935. [DOI] [PubMed] [Google Scholar]
- 125.Ledeboer A, Jekich BM, Sloane EM, et al. Intrathecal interleukin-10 gene therapy attenuates paclitaxel-induced mechanical allodynia and proinflammatory cytokine expression in dorsal root ganglia in rats. Brain Behav. Immun. 2007;21:686–698. doi: 10.1016/j.bbi.2006.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Byrd-Leifer CA, Block EF, Takeda K, Akira S, Ding A. The role of MyD88 and TLR4 in the LPS-mimetic activity of taxol. Eur. J. Immunol. 2001;31:2448–2457. doi: 10.1002/1521-4141(200108)31:8<2448::aid-immu2448>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 127.Li Y, Zhang H, Zhang H, Kosturakis AK, Jawad AB, Dougherty PM. Toll-like receptor 4 signaling in primary sensory neurons and spinal astrocytes contribute to paclitaxel-induced peripheral neuropathy. J. Pain. 2014;15(7):712–725. doi: 10.1016/j.jpain.2014.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Park HJ, Stokes JA, Corr M, Yaksh TL. Toll-like receptor signaling regulates cisplatin-induced mechanical allodynia in mice. Cancer Chemother. Pharmacol. 2014;73(1):25–34. doi: 10.1007/s00280-013-2304-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Zhang ZJ, Dong YL, Lu Y, Cao S, Zhao ZQ, Gao YJ. Chemokine CCL2 and its receptor CCR2 in the medullary dorsal horn are involved in trigeminal neuropathic pain. J. Neuroinflammation. 2012;9:136. doi: 10.1186/1742-2094-9-136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Abbadie C, Lindia JA, Cumiskey AM, et al. Impaired neuropathic pain responses in mice lacking the chemokine receptor CCR2. Proc. Natl Acad. Sci. USA. 2003;100(13):7947–7952. doi: 10.1073/pnas.1331358100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Hershman DL, Lacchetti C, Loprinzi CL. Prevention and management of chemotherapy-induced peripheral neuropathy in survivors of adult cancers: American Society of Clinical Oncology clinical practice guideline summary. J. Oncol. Pract. 2014;10(6):e421–e424. doi: 10.1200/JOP.2014.001776. [DOI] [PubMed] [Google Scholar]; • Recent review article summarizing the agents that have failed to demonstrate effective prevention of CIPN.
- 132.Anand P, Shenoy R, Palmer JE, et al. Clinical trial of the p38 MAP kinase inhibitor dilmapimod in neuropathic pain following nerve injury. Eur. J. Pain. 2011;15(10):1040–1048. doi: 10.1016/j.ejpain.2011.04.005. [DOI] [PubMed] [Google Scholar]
- 133.Ostenfeld T, Krishen A, Lai RY, et al. Analgesic efficacy and safety of the novel p38 MAP kinase inhibitor, losmapimod, in patients with neuropathic pain following peripheral nerve injury: a double-blind, placebo-controlled study. Eur. J. Pain. 2013;17(6):844–857. doi: 10.1002/j.1532-2149.2012.00256.x. [DOI] [PubMed] [Google Scholar]